|
Back to 2017 Posters
PROGNOSTIC SIGNIFICANCE OF PERITONEAL WASHINGS IN POTENTIALLY RESECTABLE PANCREATIC ADENOCARCINOMA
Neha Goel*1, Kathryn T. Chen2, Karen Ruth1, Andreas Karachristos1, John P. Hoffman1, Sanjay S. Reddy1
1Surgical Oncology, Fox Chase Cancer Center, Philadelphia, PA; 2Surgical Oncology, Harbor-UCLA Hospital, Torrance, CA
Introduction: Limited data exist on the prevalence and clinical significance of positive peritoneal cytology (PPC) in potentially resectable pancreatic adenocarcinoma. The objective of this study is to evaluate whether peritoneal cytology should be performed in pancreatic cancer and if definitive surgery, pancreatoduodenectomy (PD) or total pancreatectomy (TP), should be performed in the setting of PPC.
Methods: This is a retrospective study of 187 patients treated at our institution from 2000-2010 with the diagnosis of pancreatic adenocarcinoma who underwent peritoneal washings at the time of planned resection. Patients undergoing distal pancreatectomy (n=12), those with macroscopic disease discovered at the time of surgery (n=8), and those with stage IV disease (n=7) were excluded. Associations of peritoneal cytology on final pathologic review with margin status and pStage were also evaluated.
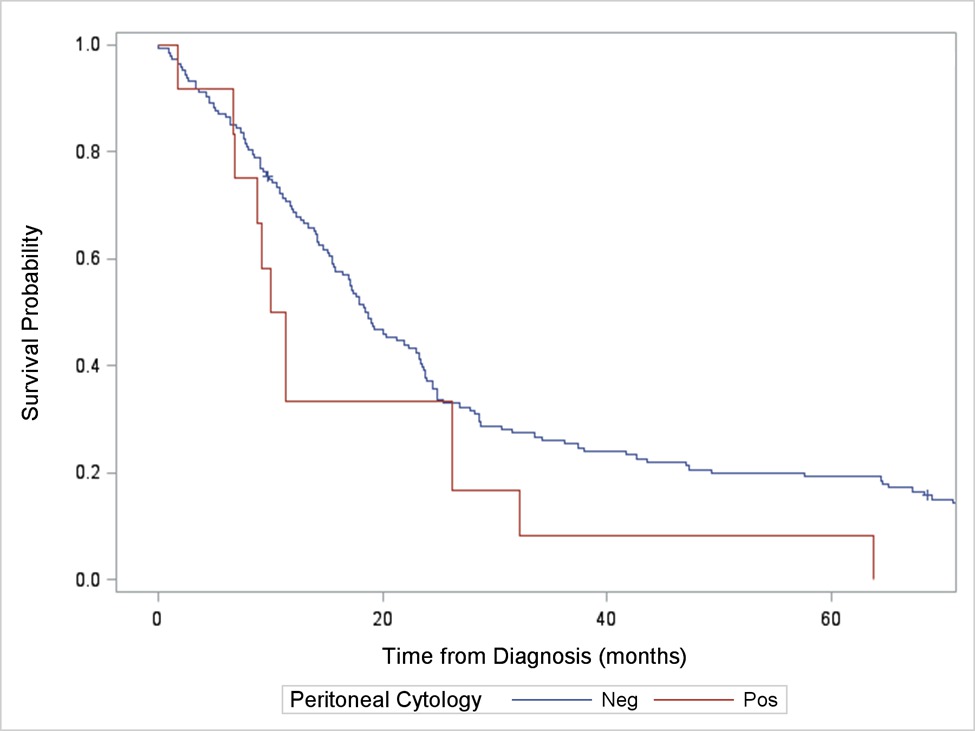
Results: After review, 160 patients met inclusion criteria. The analytic cohort was 53% female (85/160) and 7% non-white race. Median age at surgery was 68 years (range 37-91). Of the 160 patients with intraoperative cytology, 15 (9%) were found to have PPC on final cytology. Overall survival was lower in those with PPC compared to those with NPC (median survival= 16.1 mo vs 20.1 mo, p=0.040).
Twelve (80%) of the 15 patients with PPC underwent definitive surgery with either a PD or TP. Overall survival for patients who underwent definitive surgery in the setting of PPC compared to those who underwent definitive surgery in the setting of NPC was lower by 8 months and trended towards significance (median survival=10.7 mo and 18.7 mo, p=0.067).
The proportion of patients with PPC increased with increasing pStage (0% in Stage 0 to33% in stage III, trend p=0.004). Fewer R0 resections were performed in those patients with PPC (6.2% in R0 patients vs 17% in R1/R2, p=0.041).
Conclusion: Although limited data exist on the utility of peritoneal cytology in pancreatic adenocarcinoma, this study shows that patients with PPC have a statistically significant worse OS and achieve a lower R0 resection rate. Peritoneal cytology should therefore be performed as it provides clinically significant information. This study also questions the overall survival benefit of performing a PD or TP in patients with PPC. No patient with PPC and resection survived more than 64 months. Additionally, median survival was lower by 8 months in patients who underwent definitive surgery in the setting of PPC. This study concludes that PPC is a strong indicator of poor OS and suggests that these patients may more likely benefit from prolonged chemotherapy with or without pancreatic resection rather than pancreatic resection alone.
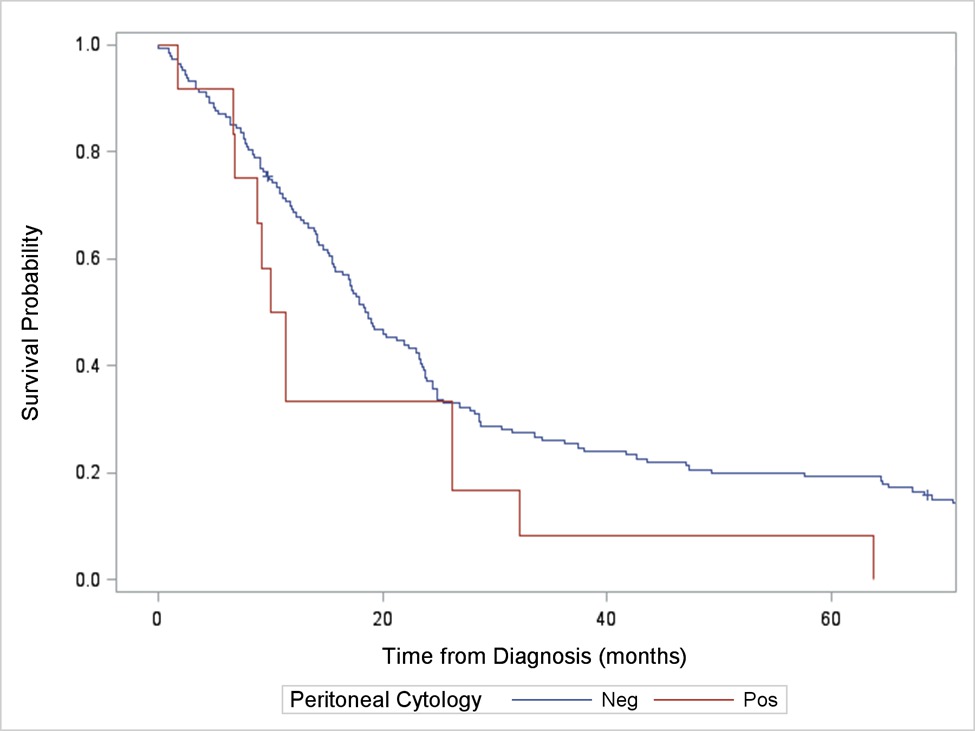
Figure 1: Kaplan-Meier survival curves for pancreatic adenocarcinoma patients with positive peritoneal cytology compared to negative peritoneal cytology (p=0.040)
Back to 2017 Posters
|