|
Back to 2017 Posters
GANGRENOUS GASTRITIS: UNUSUAL CAUSE OF UPPER GI BLEEDING
Umair Iqbal*1, Mohammad Arsalan Siddiqui2, Hafsa Anwar3, Peter Francisco1
1Internal medicine, Bassett medical center, Cooperstown, NY; 2Internal medicine, Henry Ford Hospital, Detroit, MI; 3dow university of health and sciences, Karachi, Pakistan
Introduction:
Chronic intestinal ischemia or intestinal angina is characterized by abdominal pain after meals and weight loss in elderly patients with risk factors for atherosclerosis. Here we present a case of intestinal ischemia in a patient who presented with non-specific symptoms of acute GI bleeding without abdominal symptoms.
Case:
A 67-year-old male with past medical history of COPD, atrial fibrillation on Dabigatran and coronary artery disease presents with hematemesis and black stools for a day. He reports nausea and lightheadedness but no abdominal pain, loss of appetite, postprandial abdominal pain, or weight loss. No prior history of GI bleeding. He is a current smoker with 50-year smoking history. On presentation he had BP of 146/94, pulse 83, temperature 36.6 °C, resp. rate 18. Abdominal exam was unremarkable for tenderness. Bowel sounds were present. Rectal exam revealed black stools. Labs showed hemoglobin of 16.1, hematocrit 45, platelets of 204,000, WBC of 34,000 with 83% neutrophils and bicarbonate 20 meq/L. EGD revealed stomach lumen nearly filled with subacute thrombus. Cardia revealed extensive gastric ulcer; 5-6 cm in greatest dimension, with a large visible vessel. No active site of bleeding was seen. Repeat EGD was recommended in 24 hours which revealed inflamed gangrenous-appearing gastritis throughout with multiple clean ulcers, raising suspicion for ischemia. CT angiography abdomen showed comlete proximal occlusion of SMA and near complete occlusion of celiac artery. CT also revealed hypertrophic IMA that also had ostial stenosis. Patient underwent successful SMA bypass from left iliac to mid SMA with PTFE graft. He was discharged home on aspirin daily.
Discussion:
Patients with chronic mesenteric ischemia present with recurrent abdominal pain after meals, resulting in fear of eating and weight loss. In a survey of 270 patients, weight loss, postprandial pain, adapted eating pattern, and diarrhea are associated with chronic mesenteric ischemia. Probability of diagnosis increases to 60% with all four symptoms, and reduces to 13% if none are present. Few patients present with non-specific symptoms of nausea, vomiting and/or lower GI bleeding. This patient was unique in that he had no abdominal pain even with a total occlusion of SMA, possibly due to well-formed collaterals which were seen in his CT abdomen. His upper GI bleeding was likely a result of gangrenous gastritis from ischemic bowel from total occlusion of SMA. The non-specific symptoms and unremarkable physical exam demonstrate how silently intestinal ischemia can present.
Conclusion:
Clinicians should have a high index of suspicion in diagnosing intestinal ischemia in elderly patients with risk factors for atherosclerosis as clinical presentation can be misleading. Early diagnosis can prevent morbidity and mortality associated with this serious disease.

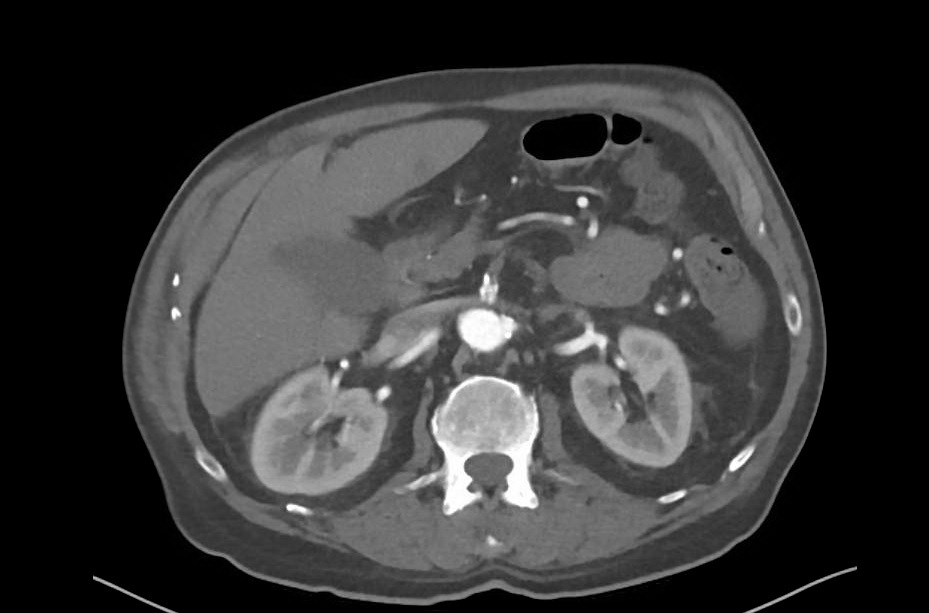
Body of stomach revealing gangrenous tissue
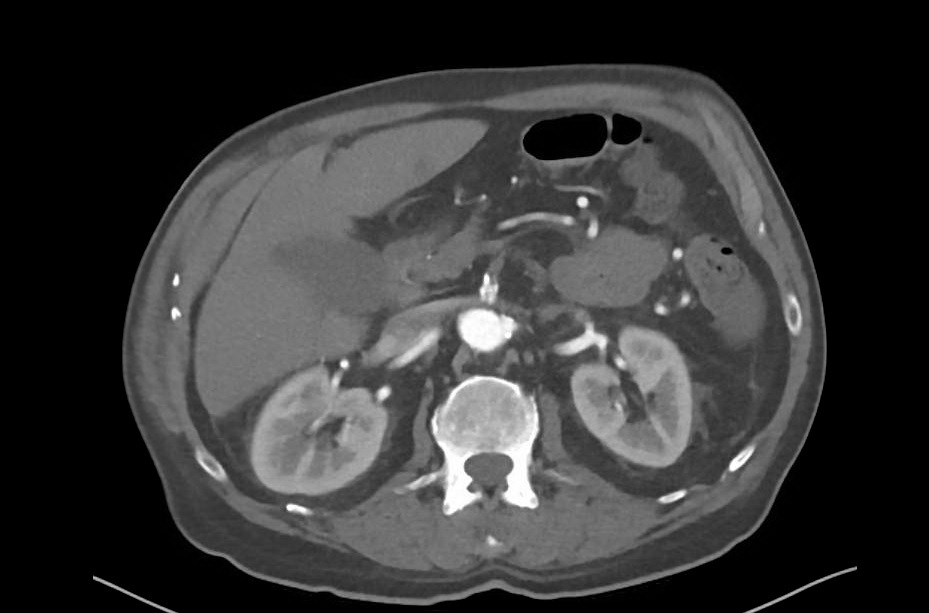
CT angiography of abdomen showing thrombosis of SMA
Back to 2017 Posters
|