|
Back to 2017 Posters
FEATURES ON HIGH-RESOLUTION ESOPHAGEAL MANOMETRY ARE PREDICTIVE OF POST-OPERATIVE DYSPHAGIA IN PATIENTS UNDERGOING LAPAROSCOPIC ANTI-REFLUX SURGERY
Kenika R. Robinson*1, Jonathan Schoen2, Frank I. Scott1, Paul Menard-Katcher1
1Medicine, University of Colorado School of Medicine, Aurora, CO; 2Surgery, University of Colorado School of Medicine, Aurora, CO
BACKGROUND
Laparoscopic anti-reflux surgery (LARS) is an effective surgical intervention for gastroesophageal reflux disease (GERD). However up to 36% of patients experience dysphagia after LARS. High-resolution esophageal manometry (HRM) is indicated for pre-operative evaluation prior to LARS to exclude an esophageal dsymotility, notably achalasia. The Chicago Classification (CC) is a validated HRM classification scheme of motility disorders. At present, there are limited data on HRM parameters that predict the development of post-LARS dysphagia (PLD).
AIM
We sought to examine pre-LARS HRM characteristics to determine factors that might predict the development of PLD.
METHODS
We conducted a retrospective study of patients undergoing LARS at a large tertiary academic medical center who had pre-operatively undergone HRM testing. The primary outcome was PLD, defined as dysphagia lasting > 3 months after LARS or requiring intervention. HRM data were assessed via version 3.0 of the CC. CC diagnoses and manometric variables were compared between subjects who did and did not develop PLD using descriptive statistics. ROC analysis was conducted for significant continuous covariates to estimate their test characteristics (sensitivity and specificity) as well as to determine an optimal cut-point via the Liu method.
RESULTS
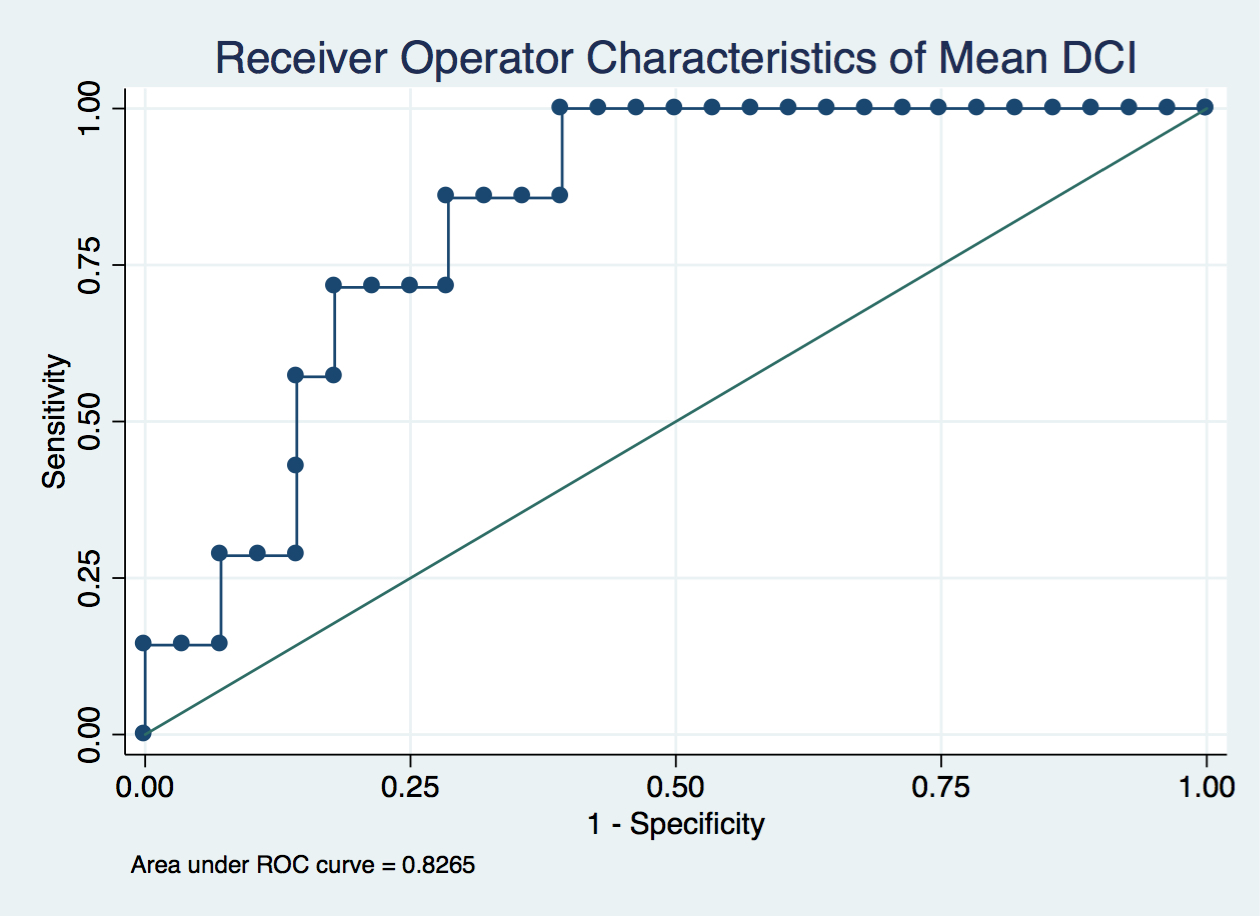
46 subjects underwent LARS during the study period (2012-16); Eight (17%) developed PLD. Of these 2 required re-operation and 3 underwent endoscopic evaluation (2 dilated). 37 subjects underwent pre-operative testing with HRM at our institution. 2 additional subjects were excluded due to insufficient follow-up. 35 subjects were included in our analysis. Demographic data is outlined in Table 1. Of the 35, 7 developed PLD. 4/7 (57%) who developed PLD met CC criteria for Ineffective Esophageal Motility (IEM) on pre-operative HRM, compared to 3/28 (11%) who did not (p=0.02). The mean distal contractile integral (DCI) was significantly lower in patients who developed PLD (512 vs 1279 mmHg-cm-sec, p<0.03). Decreasing DCI appropriately discriminated between those with PLD and those without (Figure 1, AUC 0.827). A DCI of less than 810 mmHg-cm-sec was determined to be the optimal predictive cut-off for post-operative dysphagia (sensitivity 0.86, specificity 0.71). There was no significant difference in pre-operative dysphagia, integrated relaxation pressure, intrabolus pressure or distal latency between the two groups.
CONCLUSIONS
Post-operative dysphagia was a common complication after LARS in this cohort. A CC diagnosis of IEM and the mean DCI on pre-operative HRM testing were significantly associated with the development of PLD. Our data suggests that DCI may reliably predict the development of PLD. Further studies with larger patient populations should be pursued to validate these findings.
Table 1. Baseline Demographic Data
| | Post-Operative Dysphagia (N=7) | No Post-Operative Dysphagia (N=28) | p-value | | Age (y), mean (SD) | 43.1 (22.2) | 50.8 (16.5) | 0.31 | | Male Gender (%) | 3/7 (43) | 14/28 (50) | 1.0 | | Mean Body Mass Index, (SD) | 25.4 (4.8) | 28.4 (4.3) | 0.12 |
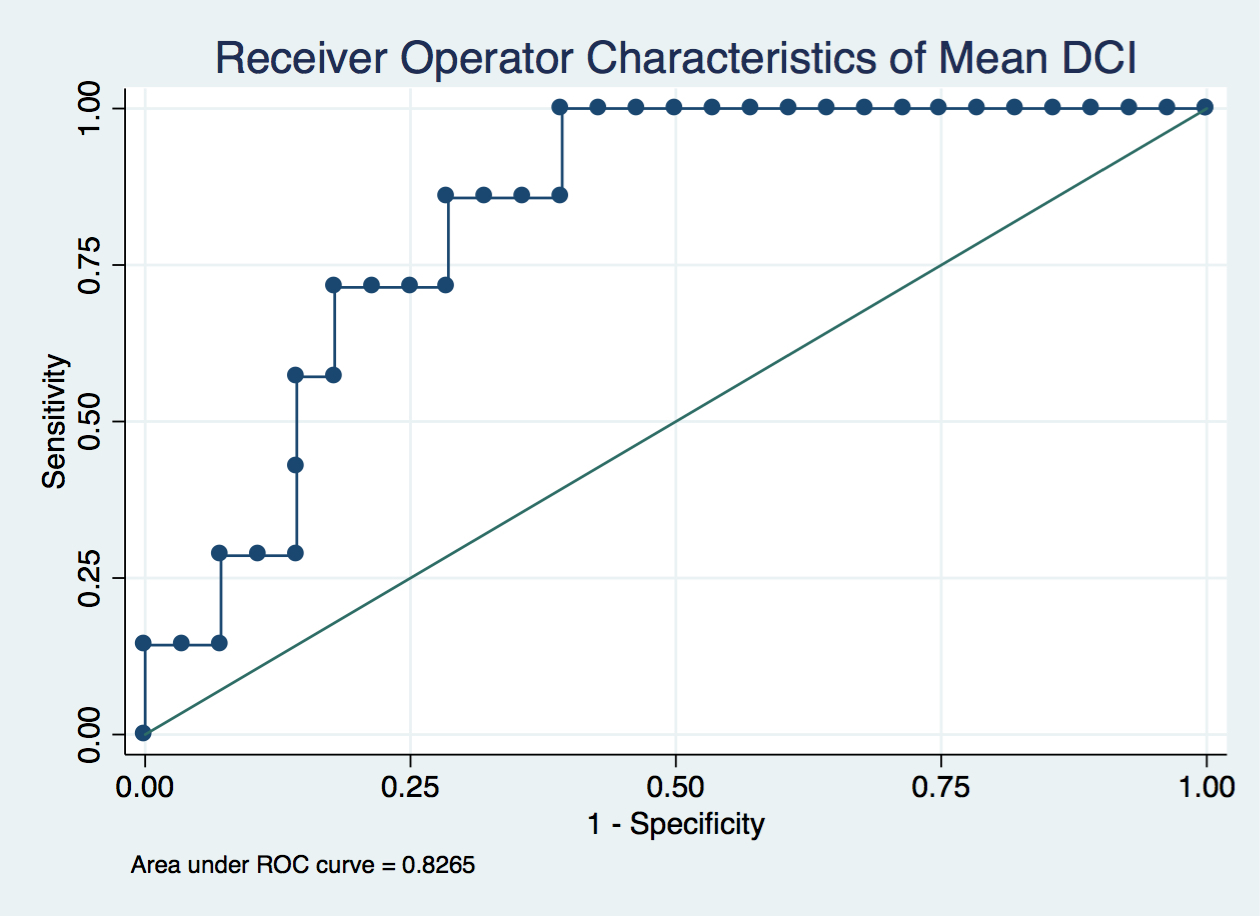 Figure 1. ROC Curve for mean DCI and post-LARS dysphagia
Back to 2017 Posters
|