|
Back to 2017 Posters
SCREENING RESULTS IN BETTER OUTCOMES EVEN IN PATIENTS WITH STAGE I RECTAL CANCER
Anne M. Dinaux*1,2, Lieve G. Leijssen1,2, Liliana G. Bordeianou1,2, Hiroko Kunitake1,2, David L. Berger1,2
1General and Gastrointestinal Surgery, Massachusetts General Hospital, Boston, MA; 2Harvard Medical School, Boston, MA
Introduction:
The implementation of population screening for colorectal cancer reduces rectal cancer incidence rates and leads to better overall long-term outcomes. However, the majority of the literature on screening does not differentiate between different AJCC stages. This study assesses whether screening leads to better outcomes in those with the best prognosis; patients with Stage I disease.
Methods:
A retrospective analysis of all non-neo-adjuvantly treated rectal cancer patients who had AJCC stage I disease on surgical pathology. Patients were retrieved from a prospectively maintained, IRB approved data repository, which contains all patients who received surgical treatment for their primary rectal cancer at a single center between 2004-2015. Short and long-term outcomes were compared between patients who were diagnosed through screening and those who diagnosed through symptoms.
Results:
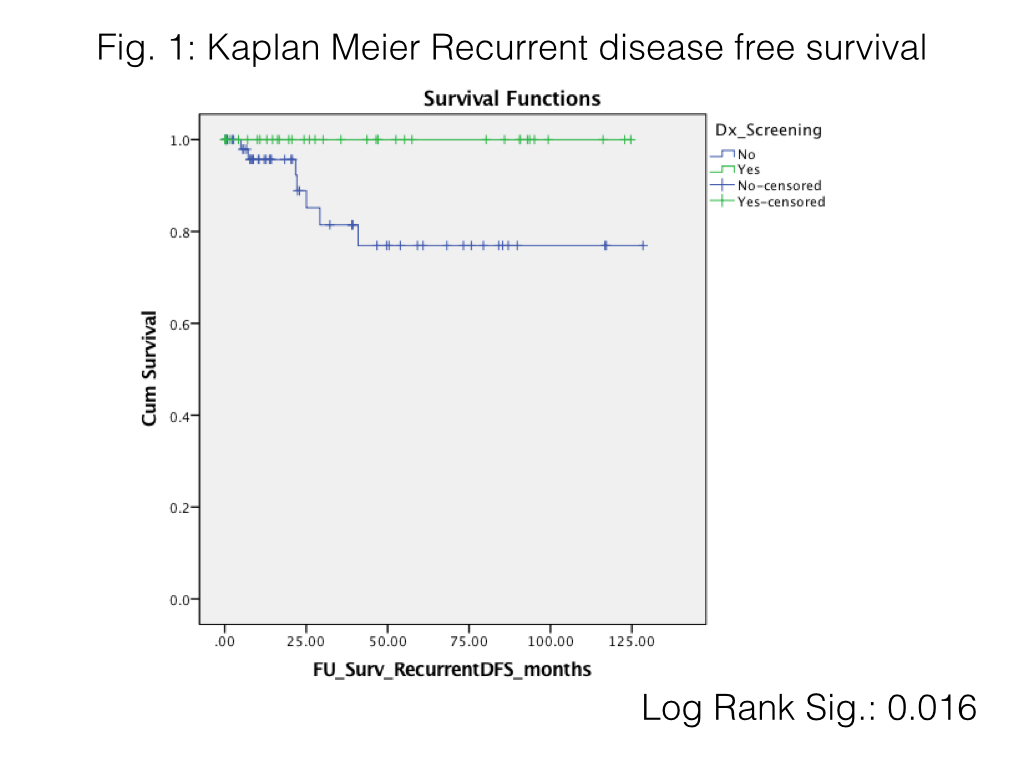
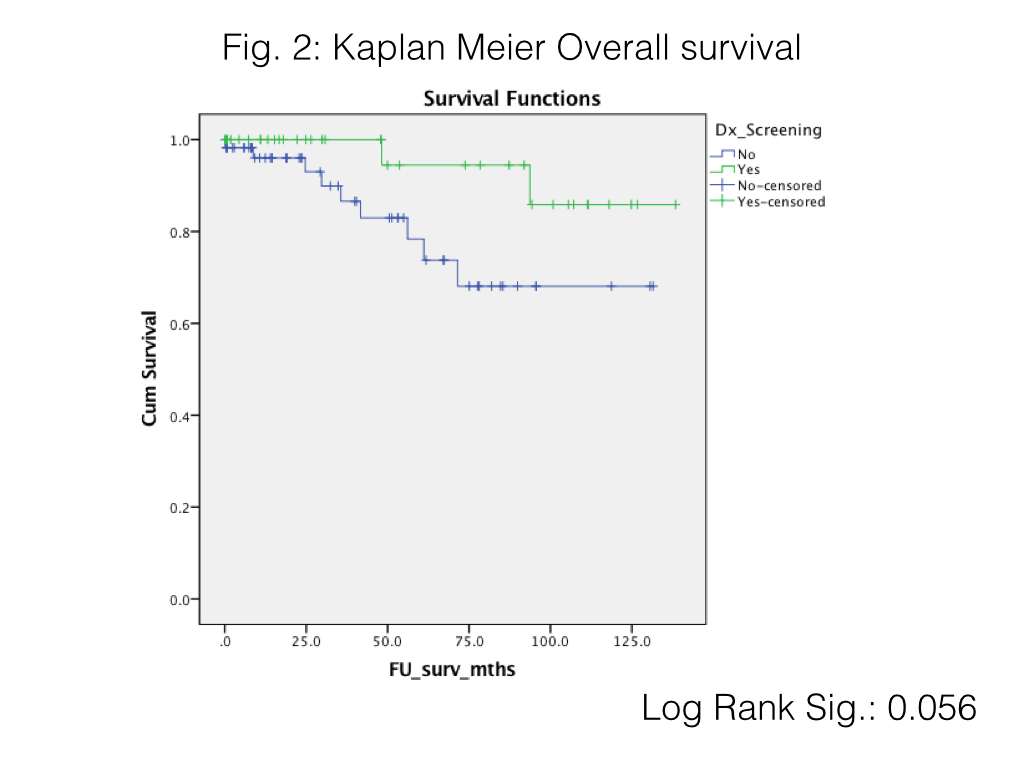
A cohort of 95 stage I patients was included, which consisted of 38 (40%) screened and 57 unscreened patients. ASA-score was significantly higher in those who were unscreened (mean 2.3 vs. 2.1; P=0.029). Depth of invasion was significantly higher in unscreened patients (rate of pT2: unscreened 42.1% vs. screened 15.8%; P=0.025), and further analysis of pathologic characteristics (EMVI, High grade disease and Large vessel/Small vessel/Perineural invasion) showed no significant differences between the two groups. None of the patients received adjuvant therapy. A total of 4 distant and 4 local recurrences occurred in the unscreened group, in contrast to no recurrences in the screened group. Thus, risk of recurrent disease was 78% higher in unscreened patients, compared to those diagnosed through screening (RR=1.78 [95%CI: 1.48 - 2.14] P<0.001). This resulted in significantly better recurrent disease free and overall survival curves for screened patients (see fig. 1 and fig. 2). There were no rectal cancer related deaths in this cohort.
Conclusions:
Stage I rectal cancer patients who were diagnosed through screening had significantly less invasive tumors and better disease free survival than patients with the same stage disease who were not diagnosed through screening. This reiterates the importance of screening and its use to not only to prevent occurrence but also improve outcomes even in patients with Stage I disease.
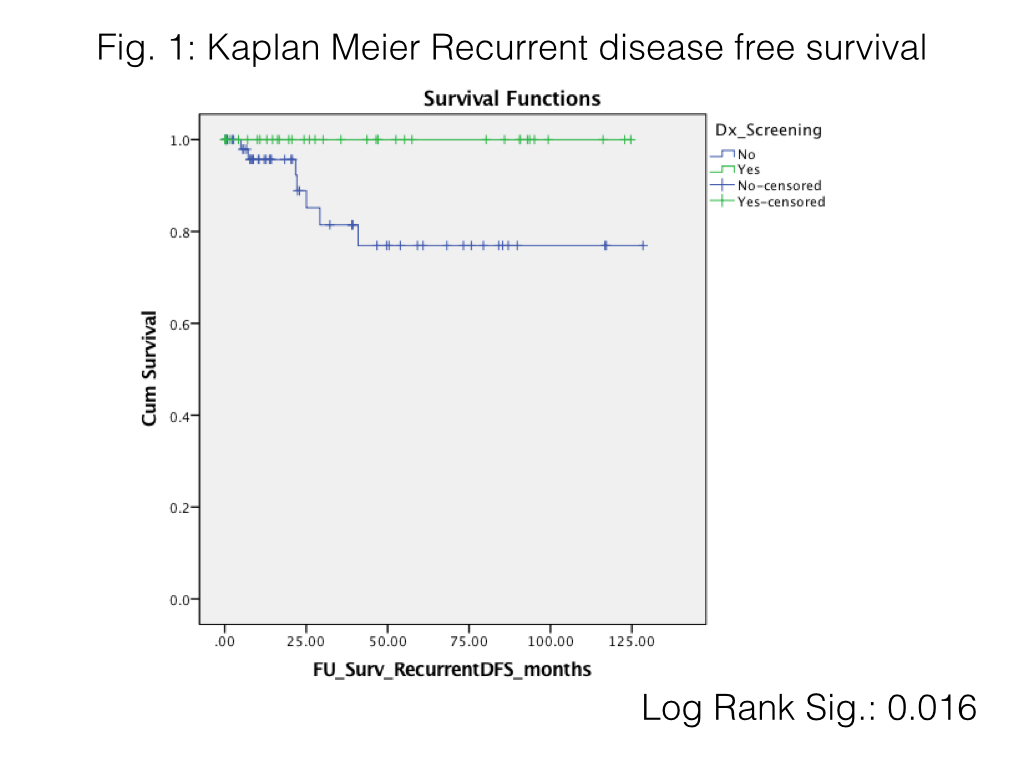
Fig. 1 Recurrent disease free survival
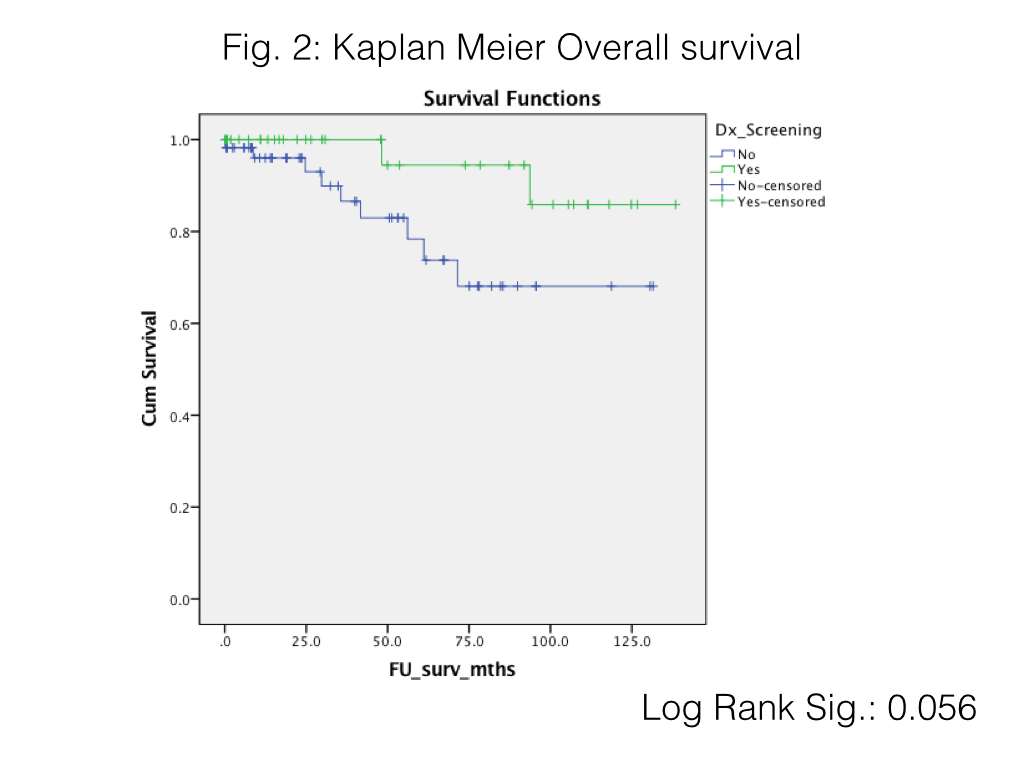
Fig. 2 Overall survival
Back to 2017 Posters
|