|
Back to 2017 Posters
ILEAL POUCH-ANAL ANASTOMOSIS FOR CHRONIC ULCERATIVE.COLITIS: INCIDENCE AND RISK FACTORS FOR 30 DAY READMISSION
Nicholas P. McKenna*1, Mohammad A. Khasawneh1, Omair Shariq1, Amy L. Lightner2, David W. Larson2, Kellie L. Mathis2
1General Surgery, Mayo Clinic, Rochester, MN; 2Colon and Rectal Surgery, Mayo Clinic, Rochester, MN
Purpose/Background: Ileal pouch-anal anastomosis (IPAA) is associated with a high risk of hospital readmission within 30 days of discharge. Risk factors for readmission are poorly understood and reasons for readmission have not been well studied. We sought to evaluate the incidence of readmission at 30 days and identify any modifiable perioperative factors for potential future intervention.
Methods/Interventions: A retrospective review of all patients undergoing either total proctocolectomy with IPAA (two stage) or completion proctectomy with IPAA (three stage) for chronic ulcerative colitis (CUC) at our institution between January 2002 and July 2015 was performed. Baseline demographics, perioperative clinical and surgical variables, readmissions, readmission diagnoses, and management of readmission were recorded. Summary, univariate, and multivariate analyses were performed.
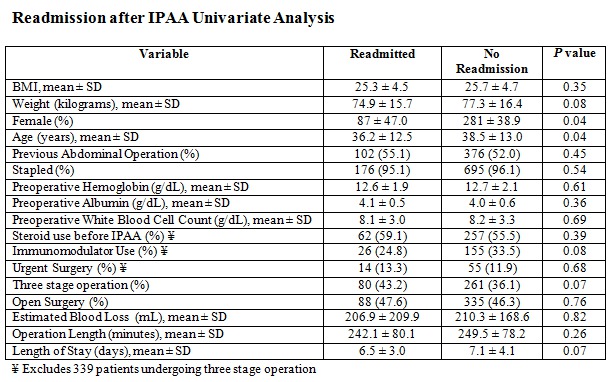
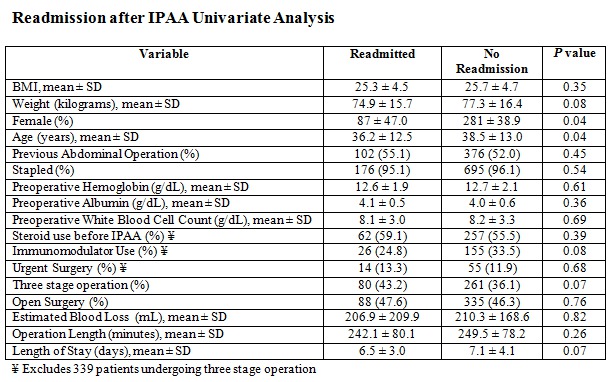
Results/Outcomes: A total of 911 patients underwent either two or three stage IPAA during the study period. 185 patients (20.3%) required readmission within 30 days with 166 (90%) requiring one readmission and 19 (10%) requiring two readmissions. This resulted in 204 readmissions with 237 diagnoses. The leading etiologies for readmission included small bowel obstruction (n = 55, 23.2%), pelvic sepsis (n = 43, 18.1%), dehydration (n=42, 17.7%), and venous thromboembolism (VTE) (n=31, 13.1%). 65.4% (n=119) of readmissions were managed medically, 19.2% (n = 35) required radiologic intervention, and 14.8% (n=27) required operative intervention. The mean (SD) readmission length of stay (LOS) was 5.9 days (±4.2) for a mean (SD) total LOS of 12.7 days (±5.8) compared to a mean (SD) LOS of 7.1 days (±4.1) for those not readmitted. On univariate analysis, younger age (readmitted mean [95% CI] = 36.2 years [34.3-38.1] versus not readmitted mean [95% CI] = 38.5 years [37.4-39.4], p = .03) and female sex (readmitted n = 87 [47%] versus not readmitted n = 281 [38.9%], p = .04) had a significantly increased risk of readmission. No other perioperative risk factors reached significance. On multivariate analysis, neither patient age (OR = 1.01; 95% CI, 1.0-1.03, p = 0.06) nor female sex (OR = 1.33; 95% CI, 0.96-1.85; p = 0.08) were independent predictors of readmission.
Conclusion/Discussion: Readmission rates following IPAA for CUC remain high. No independent risk factors for readmission were identified in our cohort. Etiologies of readmission that may be preventable include dehydration and VTE. Future areas of quality improvement could focus on education regarding stoma output and VTE prophylaxis to decrease readmission rates following IPAA.
Back to 2017 Posters
|