|
 |
Back to 2017 Posters
AMPULLARY STENOSIS AFTER ROUX-EN-Y GASTRIC BYPASS SURGERY: A NEW PHENOMENON IN THE POST-BARIATRIC SURGERY POPULATION
Andrew D. Wisneski*, Jonathan Carter, Eric K. Nakakura, Andrew Posselt, Kenzo Hirose, Lygia Stewart, Carlos U. Corvera
Surgery, University of California San Francisco, San Francisco, CA
Introduction:
Roux-en-Y gastric bypass (RYGB) surgery is routinely performed for weight loss in morbidly obese patients. At our institution, we identified a small number of patients who developed benign ampullary stenosis after previously undergoing RYGB.
Cases:
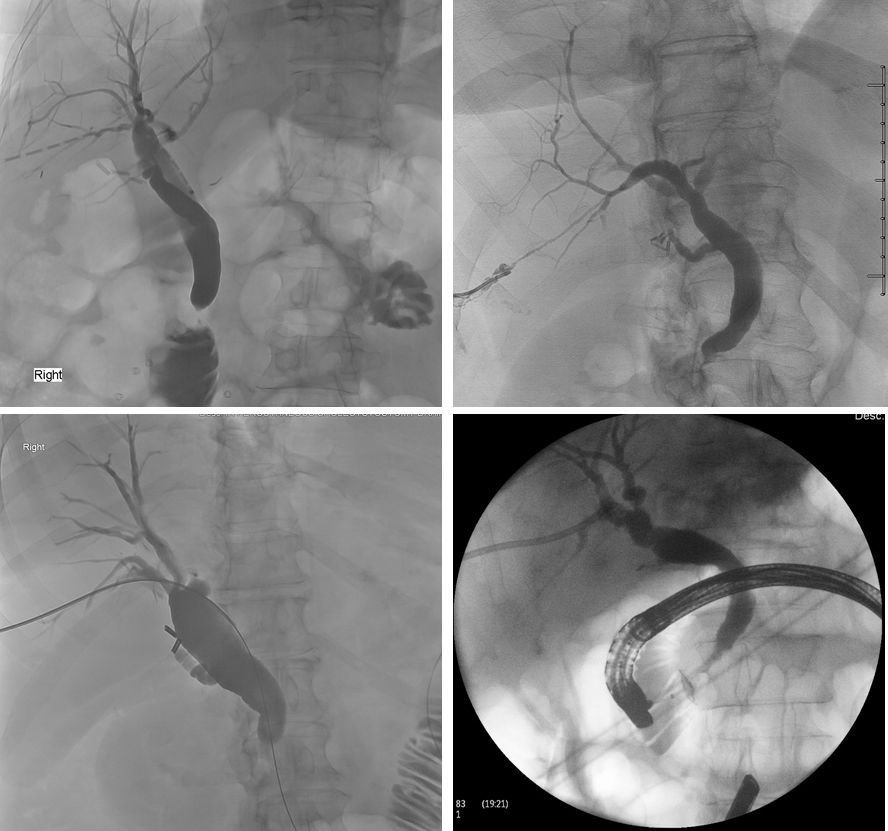
Nine patients (4 male, 5 female) with mean age 56.3±7.6 years old at presentation, had previously undergone RYGB for morbid obesity a mean 8.9±4.8 years prior to diagnosis of ampullary stenosis (Table 1). All patients had obstructive liver function test patterns and either MRCP, ERCP, or cholangiogram confirming ampullary stenosis (Figure 1). The presenting complaints/diagnoses included: abdominal pain (4 patients), back pain (1 patient), incidental finding of elevated liver enzymes (1 patient), primary sclerosing cholangitis (1 patient), and ascending cholangitis (4 patients). 5 patients had cholecystectomy prior to presentation. 2 patients (1 male, 1 female) had comorbidities of systemic lupus erythematosus (SLE), and 3 patients had hypothyroidism. 3 patients had positive anti-nuclear antibody titers, which included both patients with SLE.
Management and Outcomes:
A variety of interventions were performed to treat the ampullary stenosis. 2 patients received transduodenal ampullectomies. 2 patients received choledochoduodenostomies (one with common duct stone removal). 1 patient underwent laparoscopic assisted transgastric ERCP with sphincterotomy and common duct stone extraction. 1 patient was managed only with percutaneous transhepatic biliary drainage. 1 patient, in whom pre-operative ampullary malignancy was suspected, underwent a pylorus sparing Whipple procedure. 1 patient underwent laparoscopic cholecystectomy as an initial diagnostic maneuver for abdominal pain. 1 patient, thought to have a diagnosis of primary sclerosing cholangitis, underwent liver transplant and died from postoperative complications. Together, these interventions yielded 3 ampulla specimens which were all negative for malignancy after pathologic analysis. All other hepatobiliary and cytopathology specimens were negative for any evidence of malignancy.
Discussion:
Nine cases of benign ampullary stenosis affecting patients who have undergone RYGB are presented. We postulate that metabolic or hormonal derangements after RYGB alter ampullary physiology causing dysfunction or benign stricture formation. Another possibility is an autoimmune mechanism since several patients carried diagnoses of SLE, primary sclerosing cholangitis, and hypothyroidism. We present this case series to raise attention to the entity of benign ampullary stenosis associated with RYGB. Additional mechanistic studies are necessary to further understand the pathophysiology of this peculiar clinical phenomenon.
Patient Characteristics
| Patient | Age at Diagnosis | Sex | Year of RYGB | Presenting Symptoms/Diagnosis | Intervention and Year Performed | Relevant Pathology | Past Medical History | Notable Labs | | 1 | 54 | Female | 2012 | Epigastric pain, nausea | Transduodenal ampullectomy with sphincteroplasty, 2014 | NA | Hypothyroidism, nephrolithiasis, atrial fibrillation, hypertension, anxiety, depression | ANA positive | | 2 | 50 | Male | 2006 | Primary sclerosing cholangitis | Liver transplant, 2015 (Deceased postoperatively) | Liver biopsy: biliary obstruction, mild steatosis | GERD, hypertension, anemia | ANA positive | | 3 | 58 | Female | 2010 | Right upper quadrant pain, cholangitis | Percutaneous transhepatic biliary drain, 2014 | Benign biliary brushings | Heavy alcohol use | NA | | 4 | 73 | Female | 2009 | Weight loss, back pain, slightly elevated CA 19-9 | Pylorus sparing Whipple procedure, 2015 | Pre-op biliary brushings: malignant cytology. Ampulla (operative specimen): periampullary ulceration and fibrosis with sub-mucosal abscess. No tumor. Focal increase of plasma cells in periductal infiltrate, rare IgG4 cells. | Systemic lupus erythematosus, aortic stenosis | Pre-op CA 19-9: 37 (reference <36) | | 5 | 51 | Male | 2005 | Incidentally elevated liver function enzymes | Transduodenal ampullectomy with choledochoduodenostomy, 2016 | Ampulla: No neoplasm identified | Systemic lupus erythematosus, Raynauds syndrome, nephrolithiasis, hepatitis C, fatty liver | ANA positive | | 6 | 53 | Male | 2005 | Epigastric pain, cholangitis | Open cholecystectomy and choledochoduodenostomy, 2016 | Common bile duct margin: no high grade dysplasia or carcinoma | Dilated viral cardiomyopathy, heavy alcohol use | NA | | 7 | 63 | Male | 2007 | Cholangitis | Laparoscopic-assisted transgastric ERCP with sphincterotomy and common duct stone extraction, 2016 | Stomach (gastrotomy site): gastric tissue with serosal fibrous adhesions | Hepatitis C, hypertension, COPD, chronic pain | NA | | 8 | 49 | Female | 1997 | Cholangitis | Common bile duct exploration, common duct stone extraction, choledochoduodenostomy, 2016 | NA | Hypothyroidism, fibromyalgia, migraines, endometriosis, obstructive sleep apnea, GERD, PTSD | NA | | 9 | 56 | Female | 2006 | Abdominal pain, nausea, emesis | Laparoscopic cholecystectomy, 2016 | Gallbladder: mild chronic cholecystitis. No calculi present. | Hypothyroidism, asthma, GERD, anxiety, depression | NA |
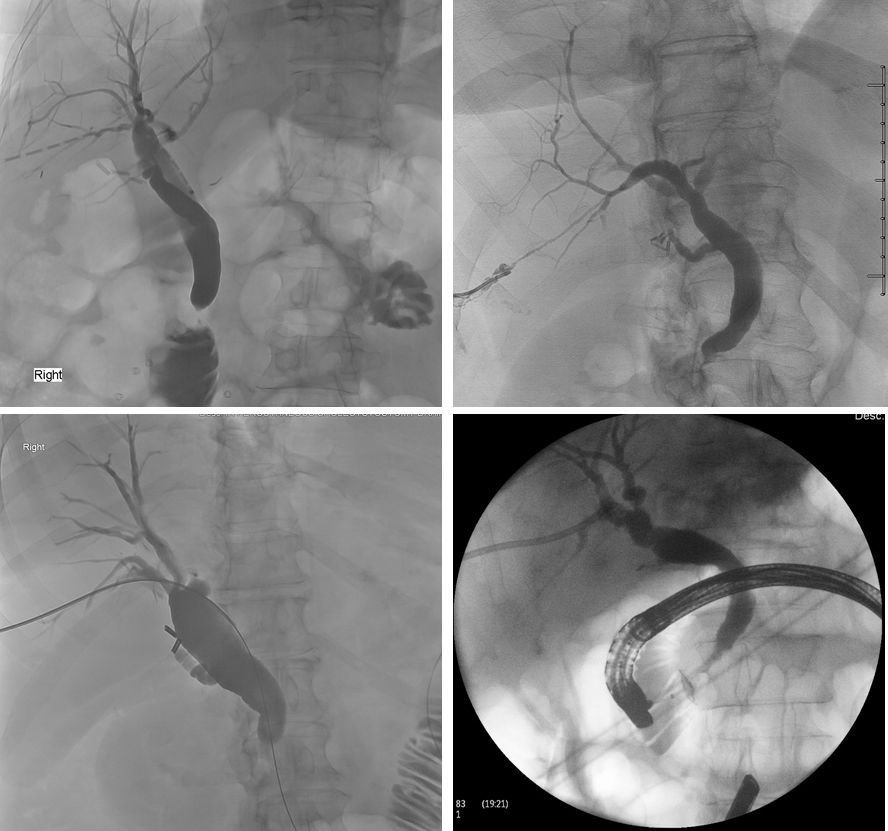 Figure 1 Figure 1: Cholangiograms (upper row and bottom left) and trans-gastric ERCP (bottom right) demonstrating ampullary stenosis.
Back to 2017 Posters
|