|
Back to 2017 Posters
AN EXPLORATION OF REGIONAL AND RURAL-URBAN DIFFERENCES IN PANCREAS CANCER SURGERY
Erin MacKinney*, Whitney Zahnd, Emily C. Sturm, Amir A. Khan, John D. Mellinger, Sabha Ganai
Southern Illinois University School of Medicine, Springfield, IL
Introduction: Current practice guidelines for pancreas cancer recommend resection at high-volume centers after multidisciplinary discussion. However, while centralization of care is promoted, there is evidence that surgery is not being recommended for a majority of patients at a national level. We hypothesized that there may be regional and rural-urban differences in resection for early-stage pancreas cancer.
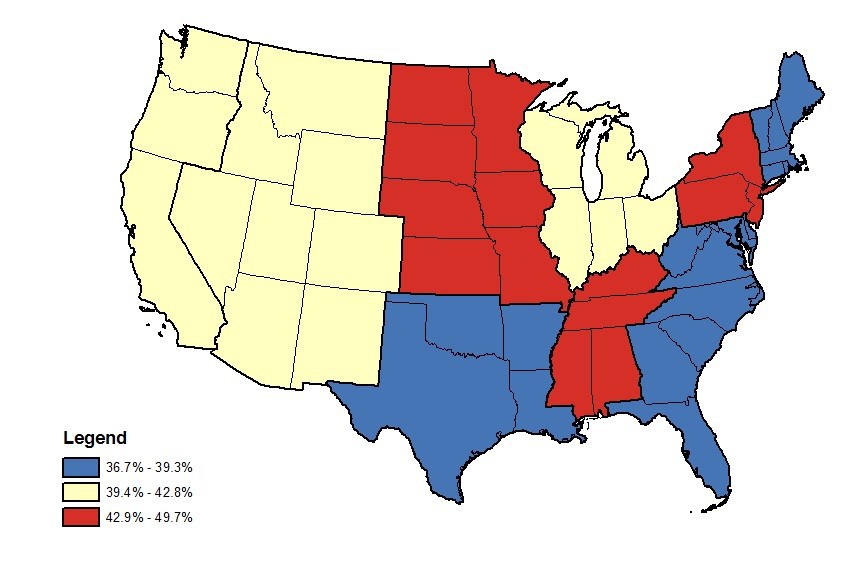
Methods: National Cancer Database pancreas cancer cases with cT1 or cT2 staging diagnosed between 1998 and 2012 with a valid rural-urban designation (n=28,451) were analyzed. The proportions of patients who had surgical resection by rural vs. urban status and region were compared. The Chi-square test for independence was used to compare the proportion of patients who had surgical resection by rural vs urban status and region, and choropleth maps were developed to display tertiles of resection by region. Cox proportional hazards analysis was used to determine rural-urban differences in survival after resection accounting for demographic, geographic, clinical, and facility characteristics.
Results: Characteristics of early stage pancreas cancer patients varied by demographic, geographic, and facility characteristics. Among cT1-T2 cancers nationwide between 1998 and 2012 (n=28,451), there were 12,486 resections (43.9%). While median distance to surgical management was different (rural 50.2 miles vs. urban 8.9 miles), resection rates were similar between rural and urban county of residence (43.8% vs. 43.9% nationally; p=0.84), except in the Middle Atlantic region where surgical resections were higher among rural patients compared to urban patients (55.3% vs. 49.1%; p=0.02). Similar median time to surgery was noted for rural and urban residence. Figure 1 demonstrates regional differences in resection rates. In adjusted analysis, there was a modest, but statistically significant increased risk for death among rural patients who underwent resection in comparison to urban patients (HR 1.11; 95% CI, 1.04-1.19, p<0.0001).
Conclusions: While cT1 and cT2 pancreatic cancers are potentially resectable, less than half of these early-stage cancers underwent surgery. There were no important differences in resection rates between rural and urban county of residence. This suggests that access disparities may not completely explain the low rates for pancreatectomy which may be a result of failure of surgical referral and ability to resect in both locales. There may also be selection bias present from differential access to Commission on Cancer accredited facilities with under-reporting of rural cases that did not undergo resection. Differences in survival after resection are present among rural patients. Further analysis of barriers to referral for pancreatic resection for rural and urban patients is warranted.
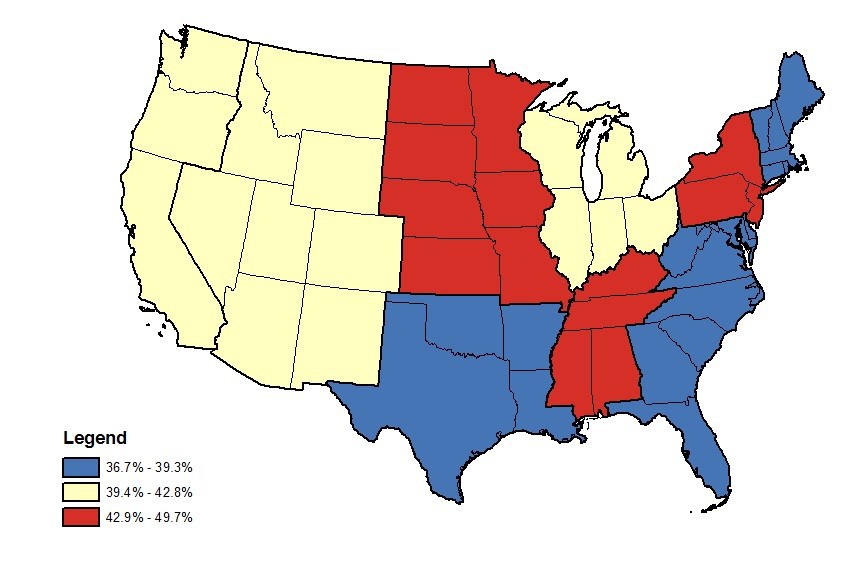
Figure 1: Regional Pancreatectomy rates for early-stage pancreas cancer; tertiles
Back to 2017 Posters
|