|
Back to 2017 Posters
SURGEON-LED IMAGING REVIEW FOR PATIENTS WITH PANCREATIC AND RELATED MASSES AND A NEW QUALITY METRIC?
Sami Tannouri*, Jessica A. Latona, Harish Lavu, Theresa P. Yeo, Jordan M. Winter, Charles J. Yeo
Surgery, Thomas Jefferson University, Philadelphia, PA
Purpose: An abundance of radiologic studies often accompanies patients at a surgical consultation. The perceived benefit of utilizing imaging as an educational tool for patients to facilitate a greater understanding of their complex medical diagnoses and enable them to actively participate in making decisions has not yet been studied.
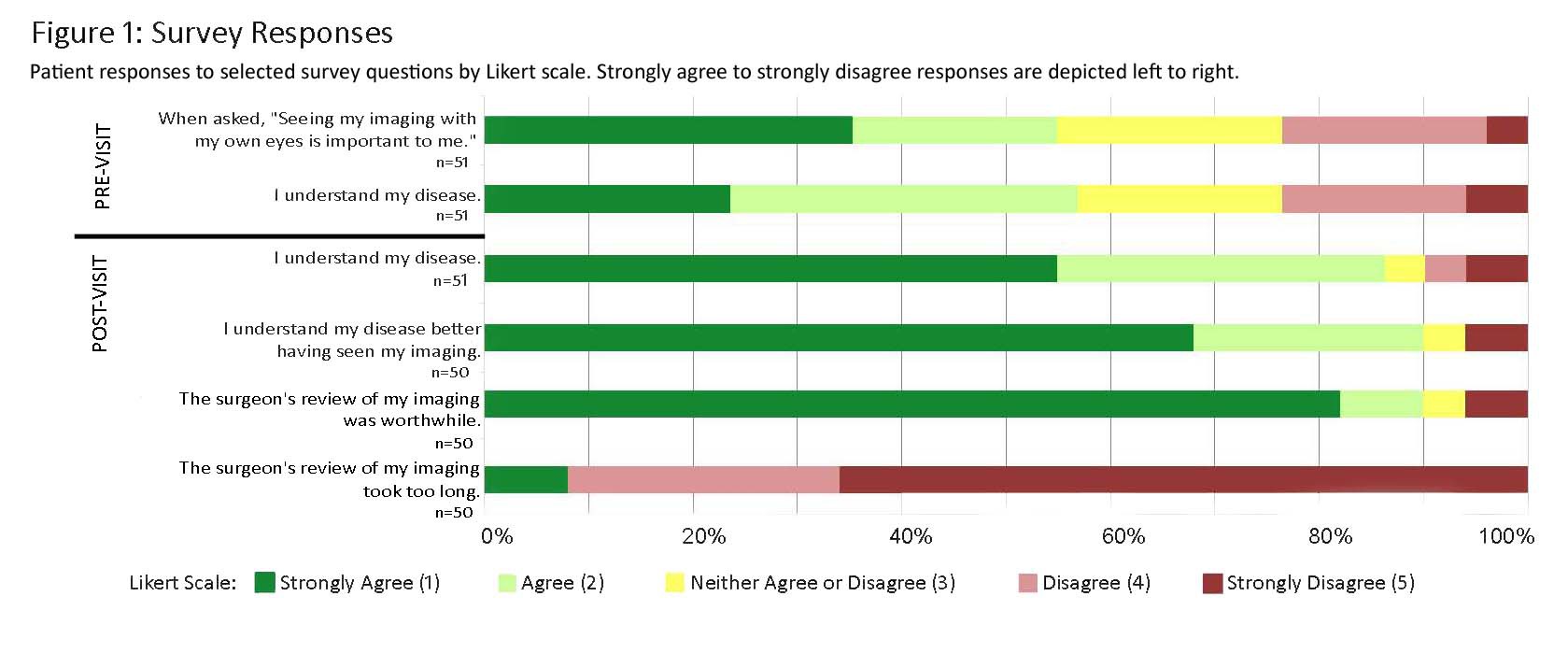
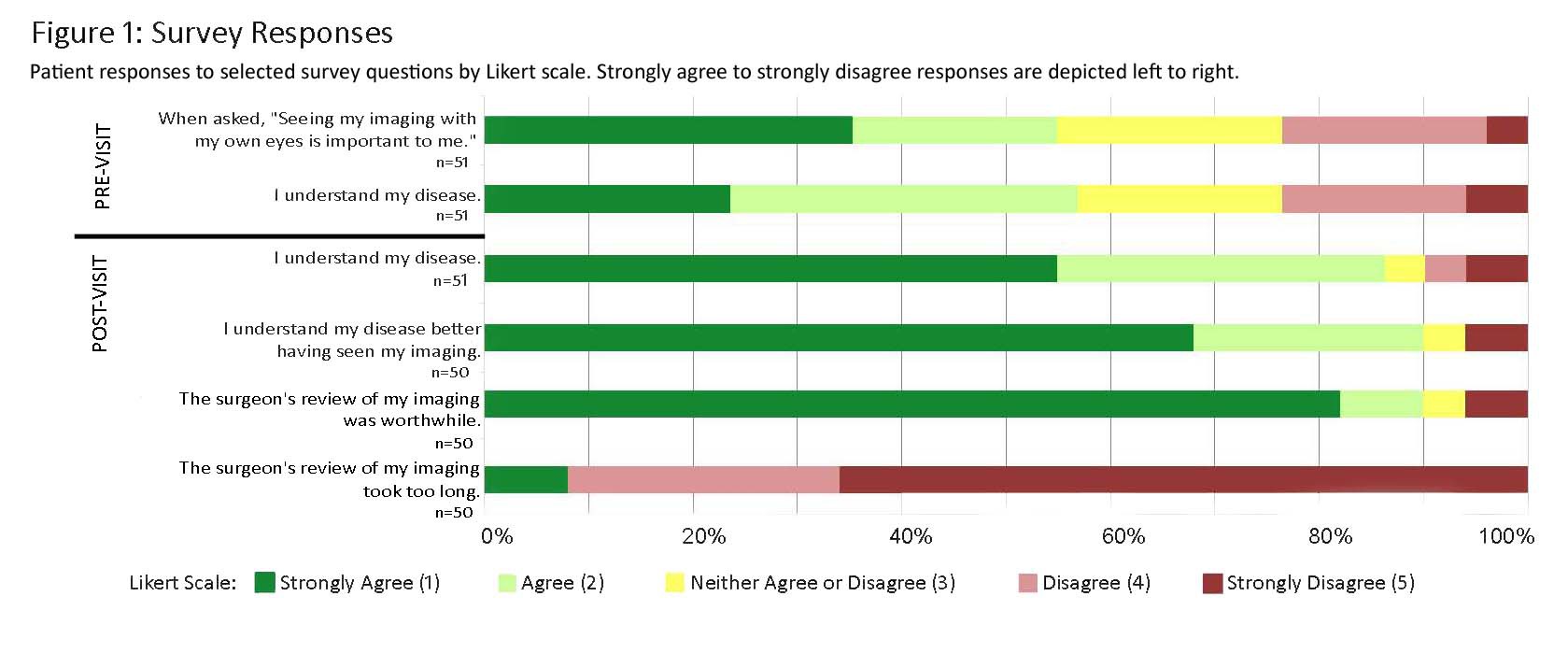
Methods: In this IRB approved study, we surveyed patients presenting for pancreaticobiliary surgical consultations at a tertiary care institution. Surveys were administered pre- and post-appointment, where a surgeon scrolled through CT and/or MRI scans with the patient and family. All scans were reviewed by our pancreaticobiliary team prior to the patient encounter. Using a 1 (strongly agree) to 5 (strongly disagree) Likert scale, patients reported their perceived importance of viewing the imaging studies and understanding of their medical condition.
Results: Of fifty-one patients surveyed, 78% reported they had not previously seen their imaging and only 55% of patients thought that it was important for them to do so. On average, the surgeons spent 2.7 ± 1.9 minutes reviewing imaging studies with the patient and family. Selected survey question responses are depicted in Figure 1. On the post-visit survey, 90% and 86% of patients, respectively, responded positively to better understanding their disease and their planned operation having seen the imaging studies. Mean scores for the statements āI understand my diseaseā and āI understand my planned operationā significantly improved from 2.5 ± 1.2 to 1.7 ± 1.1 (p = 0.001), and 3.2 ± 1.2 to 1.8 ± 0.9 (p = 0.00004) after the consultation. Ninety percent of patients felt the imaging review was worthwhile, including 100% of patients that were ultimately not deemed appropriate surgical candidates.
Conclusions: After the appointment, almost all patients felt that the imaging review with their surgeon was valuable and enhanced their understanding, although many did not have this opinion prior to the visit. Surgeons should routinely incorporate a short imaging review into patient encounters as it can be utilized as a powerful educational tool. Furthermore, in the current climate of focus on patient satisfaction, we propose that this practice be further analyzed as a possible quality metric.
Back to 2017 Posters
|