|
Back to 2017 Posters
MULTIMODAL METHOD ENDOSCOPIC CLOSURE FOR LARGE OR COMPLICATED GASTRIC FISTULAE USING THE O-O-O TECHNIQUE
Vamsi V. Alli*, Justin A. Doble, Jerome R. Lyn-Sue, Ann M. Rogers, Randy S. Haluck, Eric M. Pauli
Surgery, Penn State Milton S Hershey Medical Center, Hershey, PA
Background:
Postoperative gastric fistulae following bariatric surgery pose a difficult management problem. Multiple methods for endoscopic management have been utilized in the literature including stenting, suture plication and placement of over the scope clips (OTSC). Each of these methods poses unique technical challenges based upon the luminal anatomy and degree of angulation. We present a case series of endoscopic management of gastric fistulae using a multimodal endoscopic closure method. Our technique involves “downsizing” the defect by endoscopic suturing using and endoscopic suturing device followed by full thickness closure using an OTSC. The "O-O-O" (term derived from device names) technique allows closure of larger defects that would otherwise not be amenable to closure using OTSC methods.
Methods:
A database of all patients undergoing endoscopic closure of GI fistulae was maintained from July 2012 till present day. This database was queried for patients who underwent O-O-O closure. Patient and procedural characteristics were noted as well as outcome and length of follow-up. Patients who had resolution of clinical symptoms were not routinely reimaged following initial successful closure.
Results:
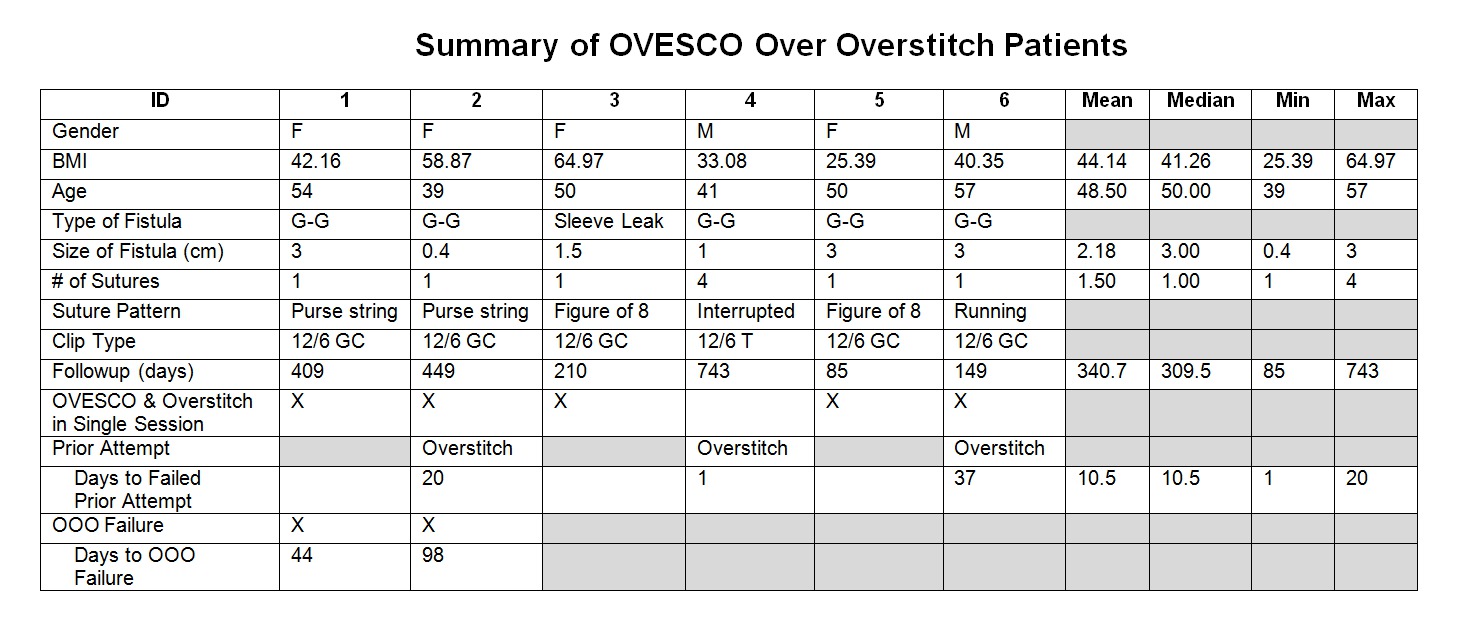
Six patients were identified who required multimodal closure for gastric fistulae. All patients had undergone bariatric surgery, 5 patients presented with gastro-gastric fistulae between their gastric pouch and remnant stomach. The 6th patient presented with multiple areas of staple line dehiscence in the subacute period following sleeve gastrectomy. 50% of patients had failed prior attempts at closure using endoscopic suturing alone. Immediate closure was successful in 100% of cases, with 2 failures (33.3%), identified at day 44 & 98 respectively. Overall success was 77.7% with a mean follow-up time of 340.8 (range 85-743) days. One of the two unsuccessful closures went on to revisional surgery.
Conclusion:
The use of OTSC alone results in immediate closure rates of 50% for with 75% sustained closure, while endoscopic suture closure results in 100% immediate closure and 23.2% sustained closure. Combining these two modalities improves both the technical feasibility of endoscopic closure and success rates for closure of gastric fistulae following bariatric surgery.
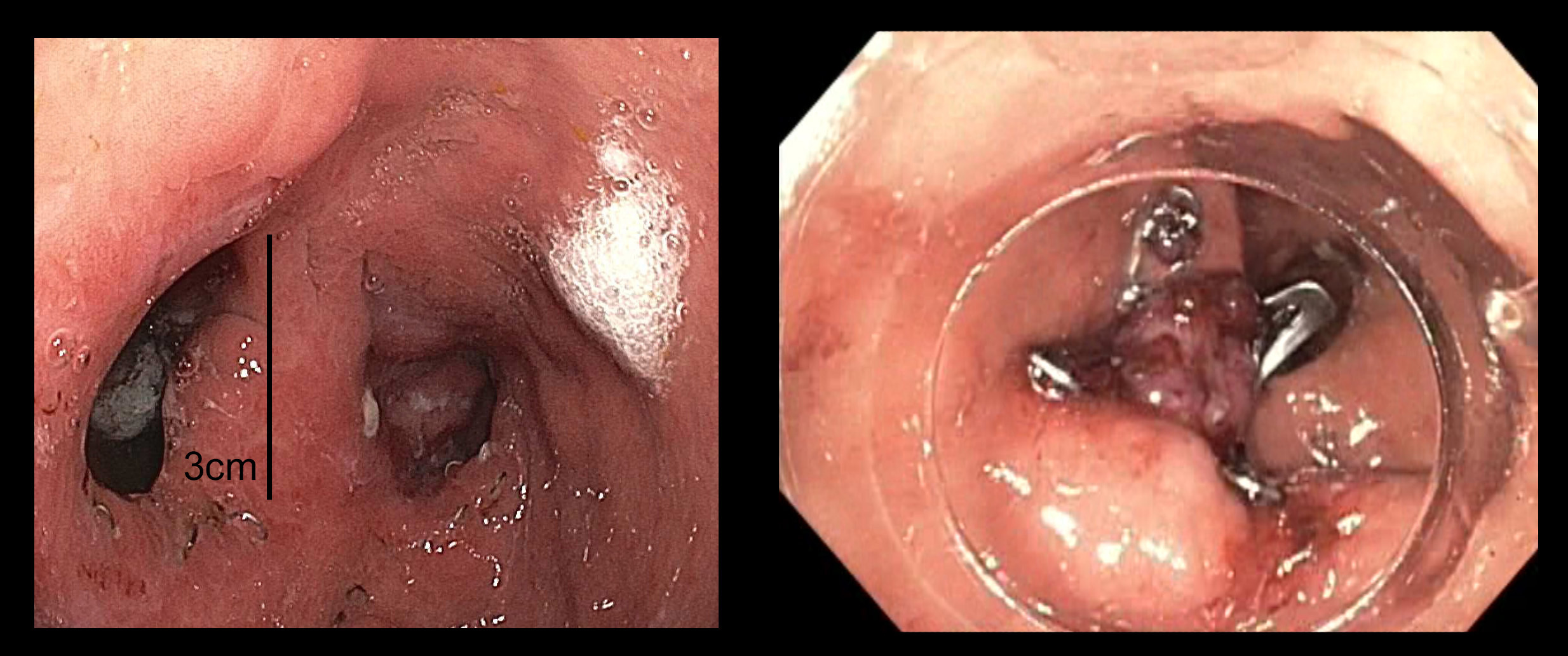
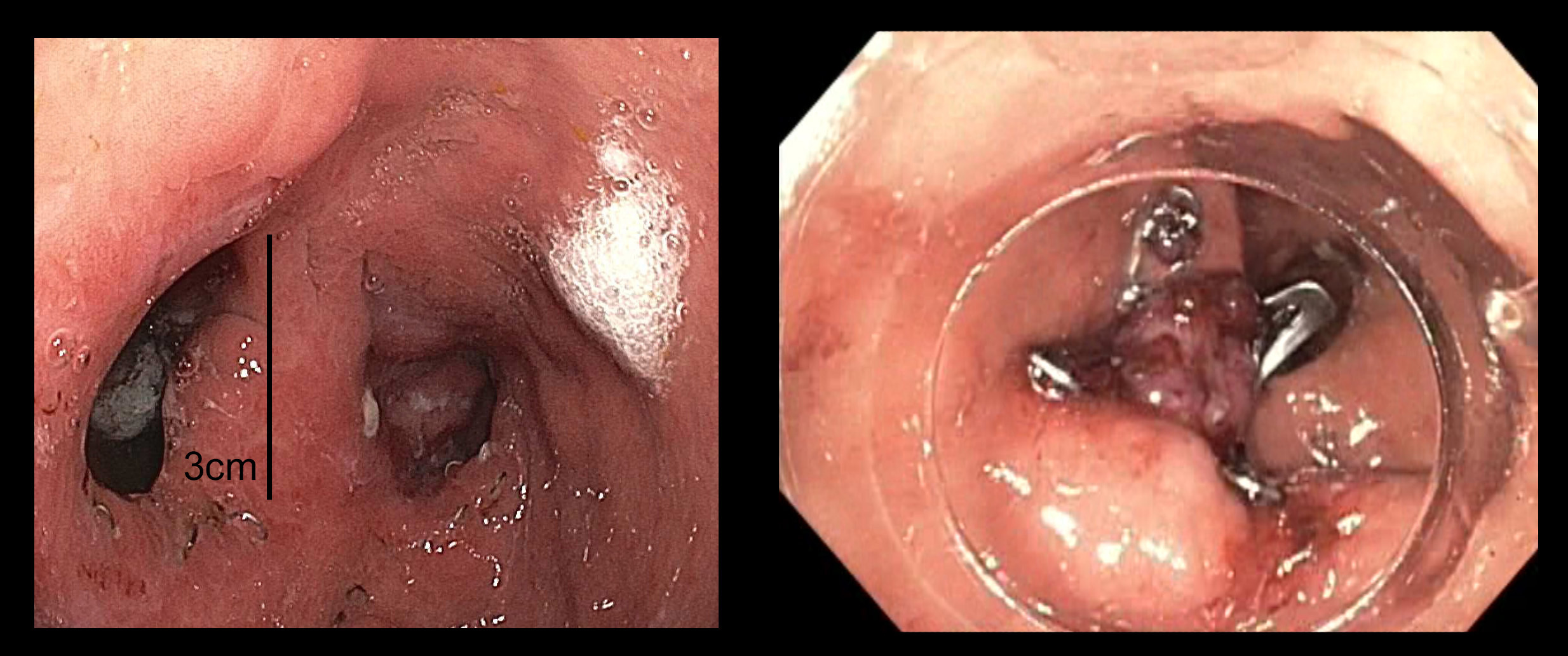
Gastrogastric fistula before and after successful closure using the O-O-O technique.
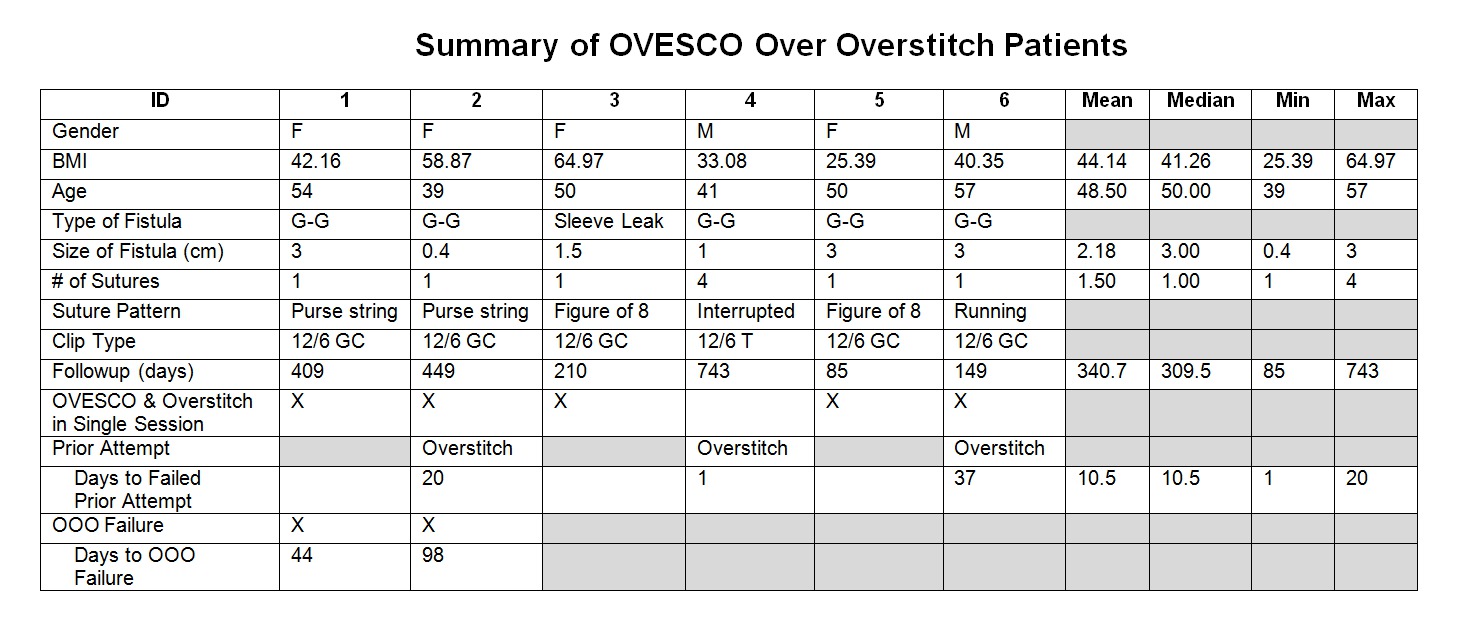
Summary table of patient and procedural characteristics.
Back to 2017 Posters
|