|
Back to 2017 Program and Abstracts
Anthropomorphic and Metabolic Outcomes Following Bariatric Surgery
Central obesity has been implicated as a risk factor in metabolic syndrome. As attention shifts from weight loss to metabolic outcomes, it is important to understand the changes in body composition following Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG). We hypothesized that improvement in anthropomorphic measurements of central obesity would be associated with improvement in metabolic status.
Methods: Retrospective analyses were performed on all patients undergoing laparoscopic SG and RYGB from 2012-2014 at a single institution. Data collected included patient demographics, anthropomorphic measurements, and status of comorbidities. Bioelectric impedance analysis (Tanita TBF-310GS) was used to estimate %fat and basal metabolic rate (BMR). Chi square, Wilcoxon Rank Sum Test, and t-tests were used where appropriate. Significance was determined as p-value <0.05.
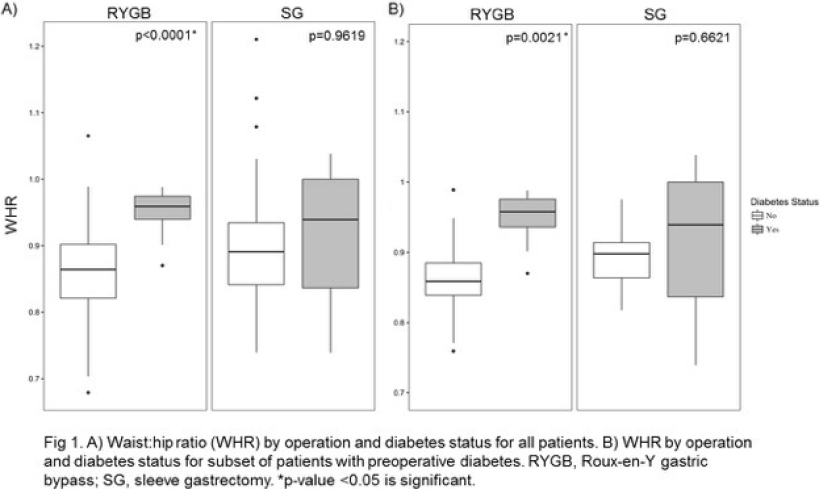
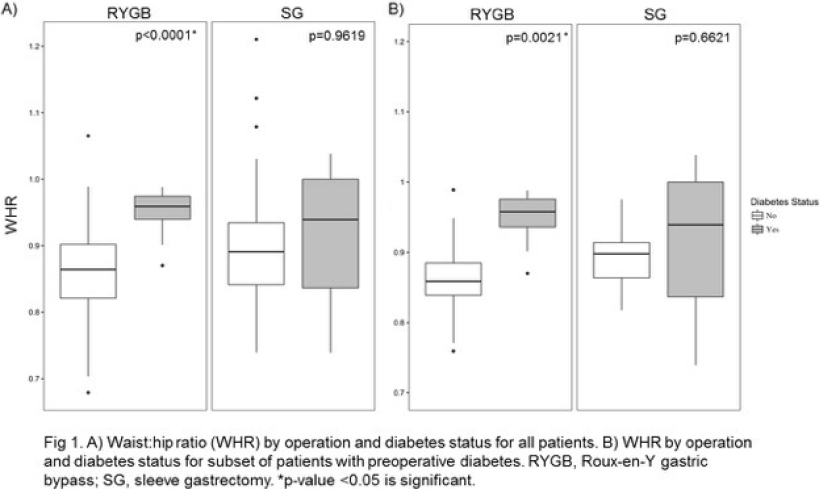
Results: There were 146 patients who met inclusion criteria. Of these, there were 79 RYGB and 67 SG patients. There were no significant differences between the two groups preoperatively. When compared to preoperative status, both RYGB and SG patients had significantly lower weight, BMI, waist and hip circumferences, %fat, and BMR. Only RYGB resulted in a lower waist:hip ratio (WHR) (p<0.0001 vs p=0.2357). When compared to each other, the RYGB group had significantly lower BMI (p=0.0419), waist (p=0.0008) and hip (p=0.0387) circumferences, and %fat (p=0.0128) as well as greater %WL (p<0.0001) and DBMI (p<0.0001) than the SG group. Although there was a trend, there was no significant difference between the groups in WHR (p=0.0672). Both groups had significant remission of diabetes and hypertension and had decreased fasting glucose postoperatively. There was a significant correlation between diabetes remission and decreased WHR (p<0.0001) in the RYGB group; this was not seen in the SG group (p=0.9619) (Fig 1A). In subset analysis only including patients with diabetes preoperatively, the significant correlation between diabetes remission and decreased WHR persisted in the RYGB group (p=0.0021) and continued to be absent in the SG group (p=0.6621) (Fig 1B).
Conclusions: Both RYGB and SG resulted in significantly improved anthropomorphic measurements and metabolic status, but only RYGB had a lower WHR. When compared to each other, RYGB resulted in a greater improvement than SG for most measurements. Remission of diabetes was correlated with decreased WHR in RYGB but not SG patients. Thus, RYGB may have the greater impact on central obesity and this may contribute to its greater metabolic impact.
Back to 2017 Program and Abstracts
|