|
 |
Back to 2017 Program and Abstracts
THE AMERICAN ASSOCIATION FOR THE SURGERY OF TRAUMA SEVERITY GRADE IS VALID AND GENERALIZABLE IN ADHESIVE SMALL BOWEL OBSTRUCTION
Matthew C. Hernandez*1, Nadeem N. Haddad1, Johnathon Aho1, Asad Choudhry1, Martin D. Zielinski1, Daniel Culliane2, Kenji Inaba3, D. D. Yeh4, Salina Wydo5, David Turay6, Andrea Pakula7, Therese Duane8, Jill Watras9, Kenneth A. Widom10, John Cull11, Carlos J. Rodriguez12, Eric A. Toschlog13, Valerie G. Sams14, John C. Graybill14, Julie A. Dunn15
1Surgery, Mayo Clinic , Rochester, MN; 2Surgery, Marshfield Clinic, Marshfield, WI; 3Surgery, LAC+USC Medical Center, Los Angeles, CA; 4Surgery, Massachusetts General Hospital, Boston, MA; 5Cooper Health System, Camden, NJ; 6Loma Linda University, Loma Linda, CA; 7Kern Medical Center, Bakersfield, CA; 8John Peter Smith, Fort Worth, TX; 9Inova Fairfax Hospital, Falls Church, VA; 10Geisinger Medical Center, Danville, PA; 11Greenville Memorial Hospital, Greenville, SC; 12Walter Reed National Military Medical Center, Bethesda, MD; 13East Carolina, Benson, NC; 14San Antonio Military Medical Center, San Antonio, TX; 15UC Health , Loveland, CO
Introduction:
The American Association for the Surgery of Trauma (AAST) anatomic severity grading system for small bowel obstruction (SBO) was validated in a single institution. We aimed to externally validate the AAST SBO grade using the Eastern Association for the Surgery of Trauma (EAST) multi-institutional SBO prospective study.
Methods:
Adults (≥18) with adhesive SBO were included. Baseline demographics, physiologic parameters (heart rate, blood pressure, respiratory rate), labs (lactate, hemoglobin, creatinine, leukocytosis), imaging findings, operative details, durations of stay, complication (Clavien-Dindo class) were collected. AAST grades were assigned by two independent reviewers based on operative findings.
Results:
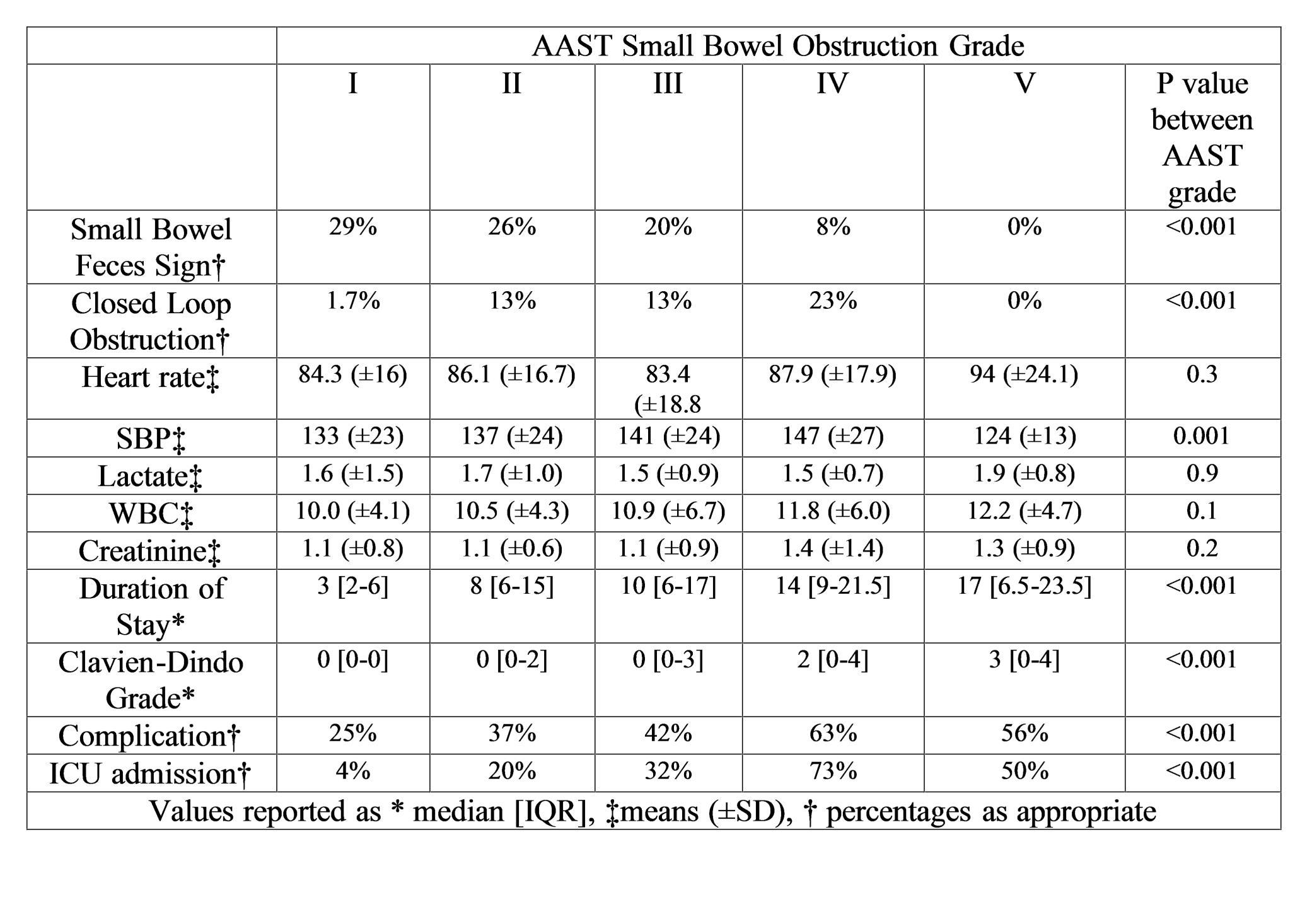
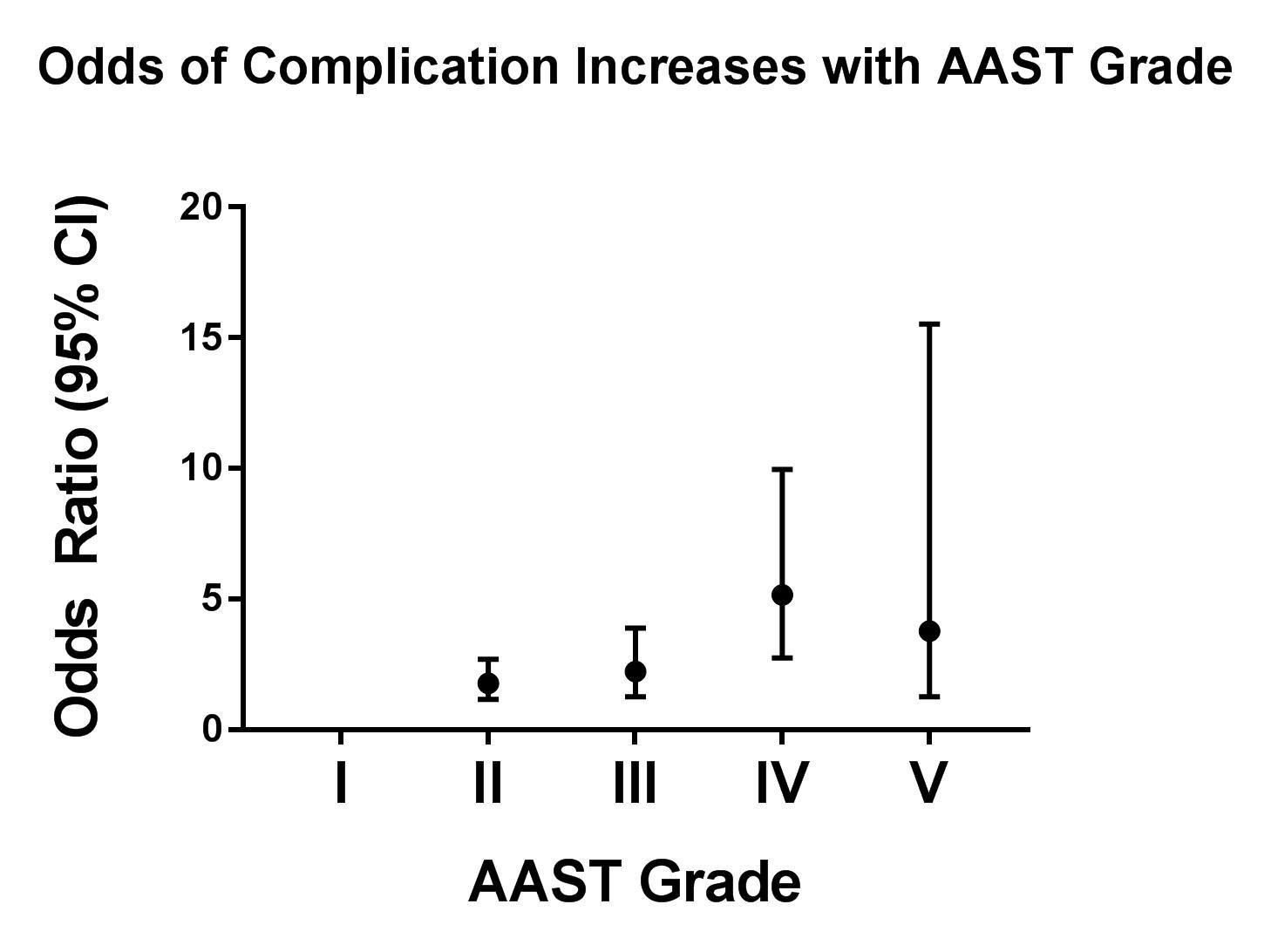
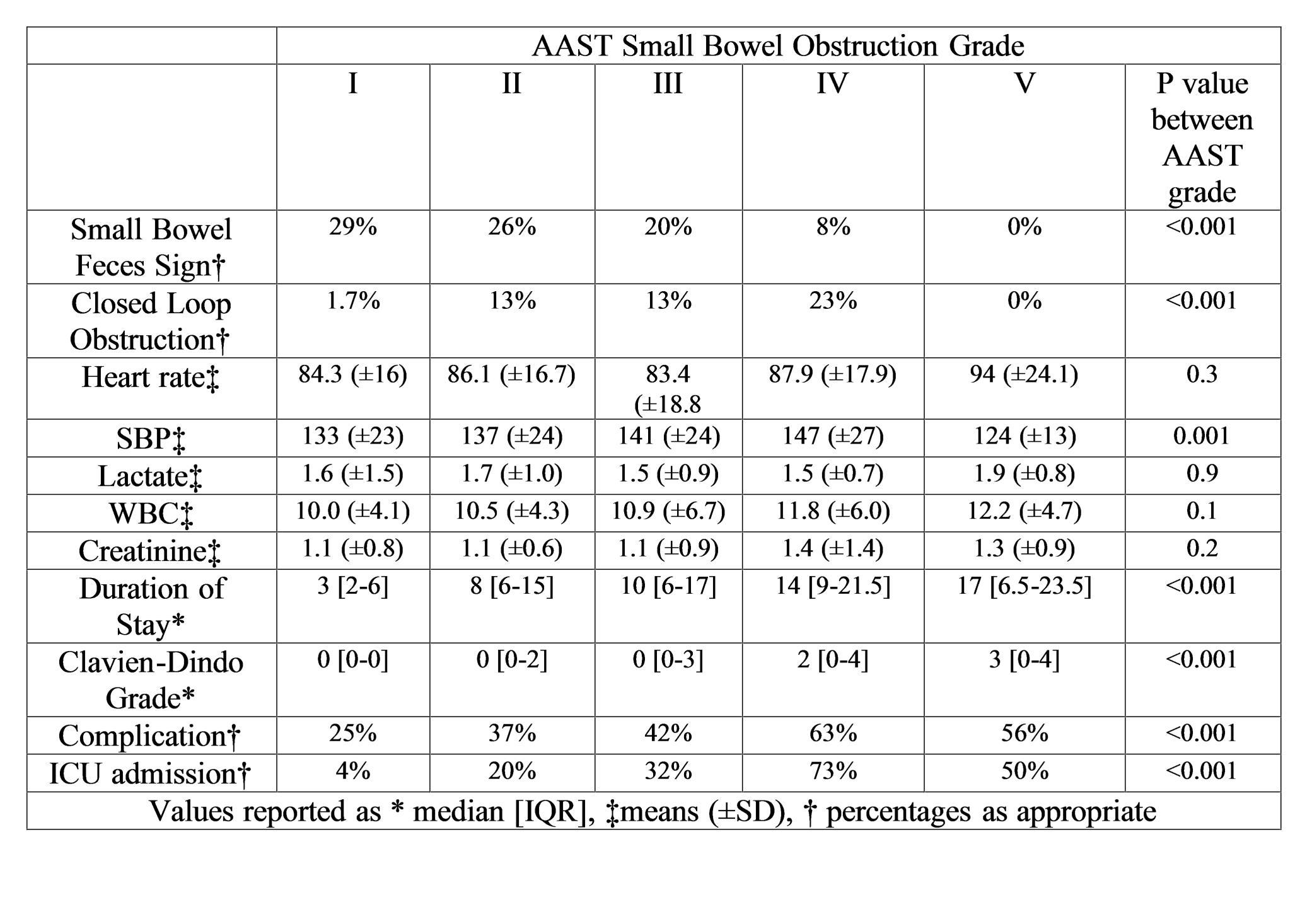
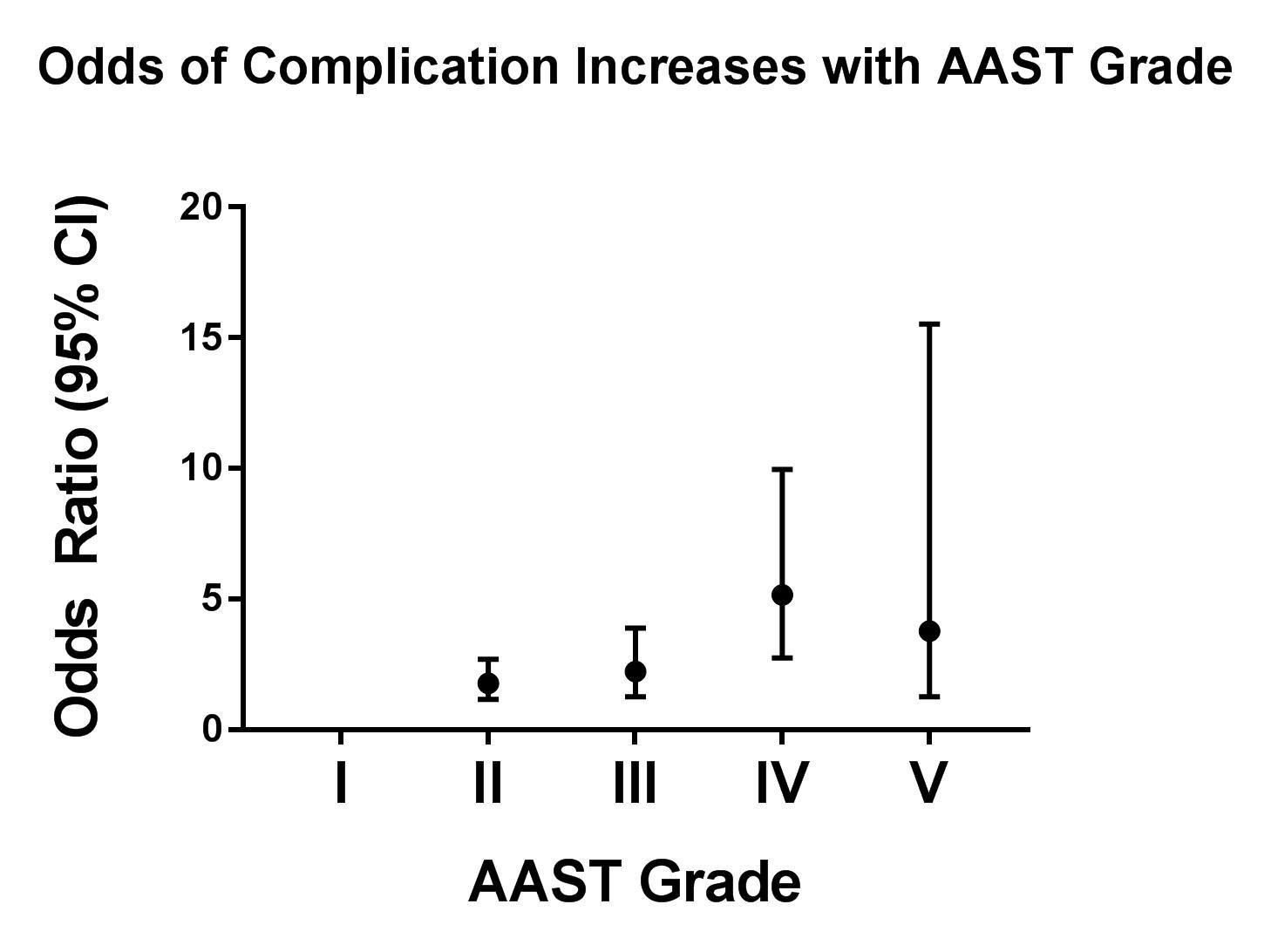
There were 638 patients with a mean (±SD) age of 61±17.8 years, 50.3% female, and mean BMI of 27.5±8.1. The AAST grades in this cohort were: Normal (n=3, 0.5%). Grade I (n=386, 60.5%), Grade II (n=135, 21.2%), Grade III (n=59, 9.2%), Grade IV (n=46.2, 7.2%), Grade V (n=9, 1.4%). Initial management included: non-operative (n=388; 61%), laparotomy (n=200, 31.3%), laparoscopy (n=13, 2.0%), and laparoscopy converted to laparotomy (n=37, 5.8%). An increased median [IQR] AAST grade was associated with need for conversion to an open procedure (2 [1-3] vs 3 [2-4], p=0.008), small bowel resection (2 [2-2] vs 3 [2-4], p<0.0001), post-operative temporary abdominal closure (2 [2-3] vs 3 [3-4], p<0.0001), and stoma creation (2 [2-3] vs 2.5 [2-4], p<0.0001). Increasing AAST grade was associated with increased anatomic severity noted on imaging findings, systolic blood pressure variability, longer duration of stay, need for intensive care, increased rate of complication and higher Clavien-Dindo complication grade (Table).
Conclusion:
The AAST SBO severity grading system has predictive validity for important clinical outcomes and allows for standardization across institutions, providers, and future research focused on optimizing preoperative diagnosis and management algorithms.
Back to 2017 Program and Abstracts
|