|
|
Back to 2017 Program and Abstracts NATIONAL DISPARITIES IN SURGICAL MANAGEMENT AND RECEIPT OF NEOADJUVANT THERAPY AMONG BLACKS WITH RECTAL CANCER: IMPLICATIONS ON OVERALL SURVIVAL Michael A. Sundberg*2, Lauren Marsh2, Sabha Ganai1,2 1Department of Surgery, Southern Illinois University, Springfield, IL; 2Epidemiology, Harvard T.H. Chan School of Public Health, Boston, MA
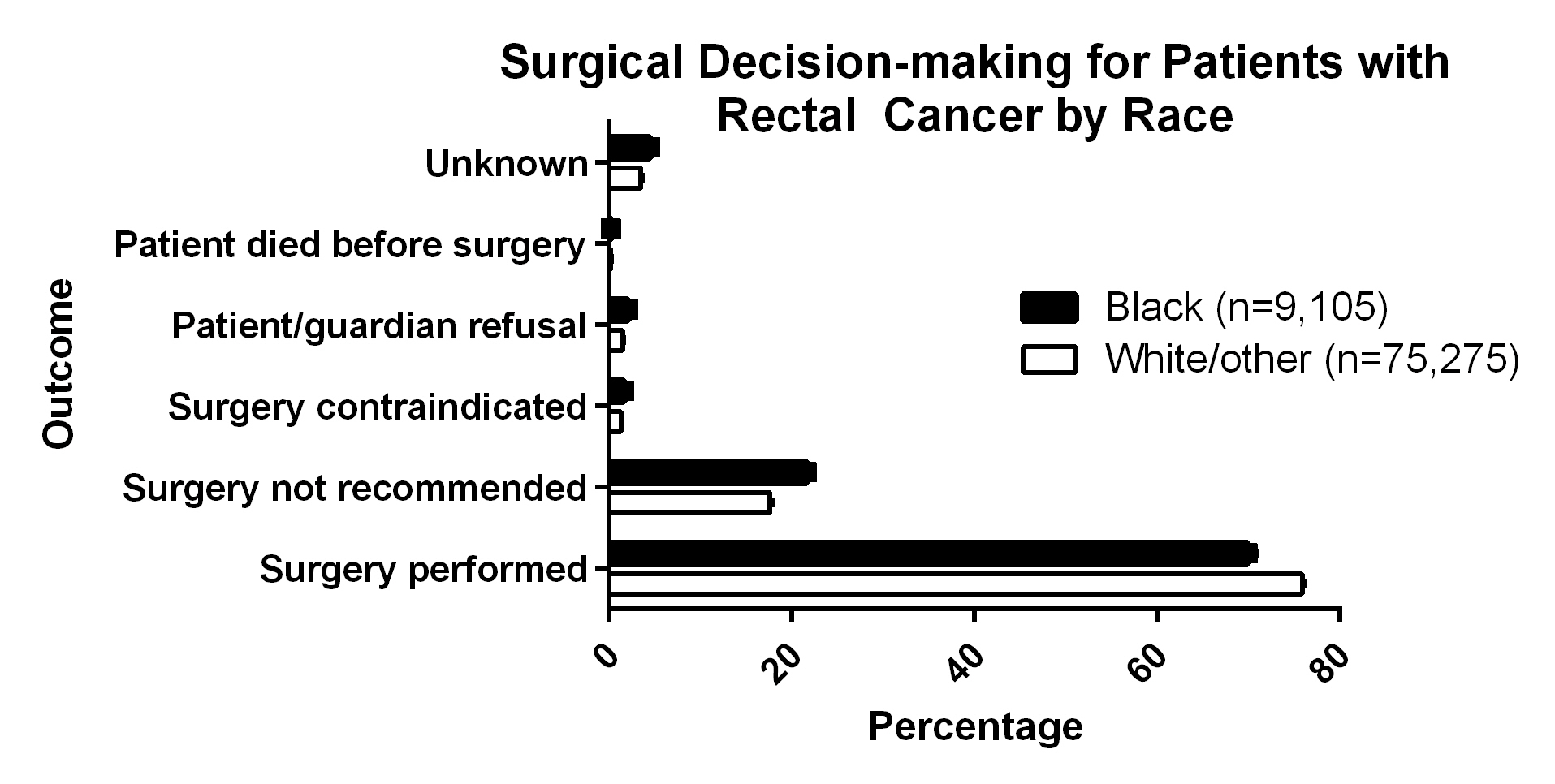
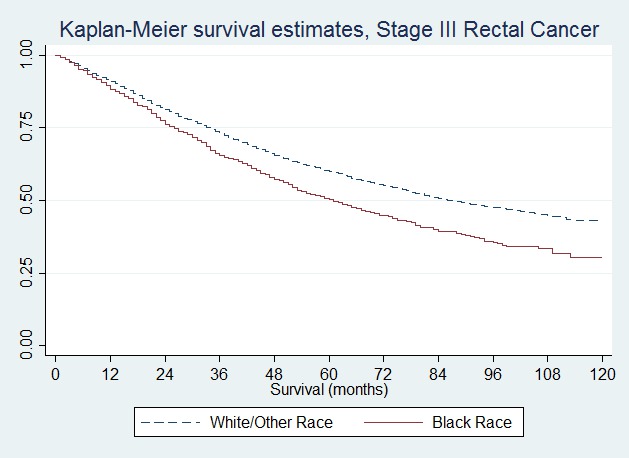
Introduction: Advances in the surgical management along with increased utilization of neoadjuvant therapy are associated with improved outcomes for rectal cancer. However, recommended therapies may not be offered consistently when diagnosed, particularly among minorities. We hypothesized that differences in utilization of surgical therapy and neoadjuvant radiation would be seen among blacks and this would impact survival. Methods: We utilized the Surveillance, Epidemiology, and End Results (SEER) database to examine 84,380 adults with rectal cancer diagnosed between 2004-2013, excluding individuals without microscopically-confirmed tissue diagnosis or with a synchronous colon cancer. Cases were dichotomized into black or non-black racial identity, with outcomes analyzed including surgical treatment and receipt of neoadjuvant radiation therapy. Multivariate logistic regression was performed to examine the likelihood of local excision and proctectomy [low anterior resection (LAR), abdominoperineal resection (APR), or exenteration] by race controlling for baseline demographics and pathologic features. Cox proportional hazards analysis was used to examine independent predictors of overall survival. Results: Blacks comprised 9,105 (10.8%) patients with rectal cancer, with significant differences in presentation by baseline demographics when compared with whites (78.2%) and other (9.6%) races (p<0.001). Pathologic stage was significantly different, with 19.0% of blacks presenting with metastatic disease, compared to 15.9% of non-blacks (p<0.001). Blacks had significant differences in surgical management (p<0.001), with higher rates of local excision (30.7% versus 23.0%), and lower rates of LAR (28.7% vs. 38.8%), and APR (9.0% vs. 12.4%). Blacks also had lower receipt of neoadjuvant radiation therapy for stage III disease (44.9% vs. 48.7%; p<0.001). Significant differences were also noted in reasons for not having surgery (p<0.001; Figure 1). When controlling for demographics, stage, grade, and use of neoadjuvant radiation therapy, the use of local excision was higher among those with black racial identity (adjusted OR 1.37; 95% CI, 1.22-1.53) while use of proctectomy was lower (adjusted OR 0.70; 95% CI, 0.64-0.77). Decreased median survival was noted for blacks (Stage III - 69 vs.87 months; Figure 2), with a hazard ratio of 1.24 (95% CI, 1.17-1.31) when controlling for demographics, stage, grade, receipt of radiation therapy, and proctectomy. Conclusions: These data suggest that there are important differences in treatments offered for rectal cancer among individuals in the United States who identify as black as compared to those who do not, with implications on overall survival. Further work on the part of healthcare delivery systems must include identifying gaps preventing delivery of appropriate neoadjuvant therapy and surgery to this minority group. Back to 2017 Program and Abstracts |
||||||||||||
© 2026 Society for Surgery of the Alimentary Tract. All Rights Reserved. Read the Privacy Policy.