|
Back to 2017 Program and Abstracts
DUODENAL CANCER IN PATIENTS WITH FAMILIAL ADENOMATOUS POLYPOSIS HAS A BETTER PROGNOSIS COMPARED TO SPORADIC NON-PAPILLARY DUODENAL CANCER
Maitham A. Moslim*1, Toms Augustin1, Andrew Tang1, Eric B. Schneider2, R Matthew Walsh1
1Department of HPB Surgery, Cleveland Clinic Foundation, Cleveland, OH; 2Department of Surgery, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA
BACKGROUND: The outcomes of surgical management of duodenal cancer in the setting of Familial Adenomatous Polyposis (FAP) disease compared to sporadic non-papillary malignancy have never been reported.
METHODS: With IRB approval, the departmental database was interrogated to identify all patients who underwent surgical treatment of sporadic non-ampullary duodenal cancer, and FAP associated duodenal cancer. The presentation, management, surgical pathology and follow-up were analyzed.
RESULTS: 48 patients with sporadic non-papillary and 12 patients with FAP duodenal cancer were identified between April 2000 - November 2014. Preoperatively no difference was encountered in gender distribution (male: 54% vs 50%; p 0.80). FAP cancer patients were diagnosed at younger age compared to sporadic (median 52.4 vs 66.5 years old; P<0.001). However, only half of FAP patients were known to have cancer preoperatively. Intraoperatively, patients with sporadic cancers underwent Whipple procedure predominantly (94%) compared to 67% of FAP related cancers. Two of FAP group had segmental duodenal resection for distal duodenal cancers, and one had pancreas sparing duodenectomy for unsuspected malignancy. Overall, sporadic cancer patients were noted to have a more advanced stage (p<0.05) on final pathology. Postoperatively 25% of FAP patients received adjuvant treatment compared to 56% of sporadic cancer patients (p 0.006). Postoperatively there was no statistically significant difference in pancreatic fistula (p 0.06), anastomotic or bile leak, deep organ space infection, delayed gastric emptying, length of stay or 30 days mortality.
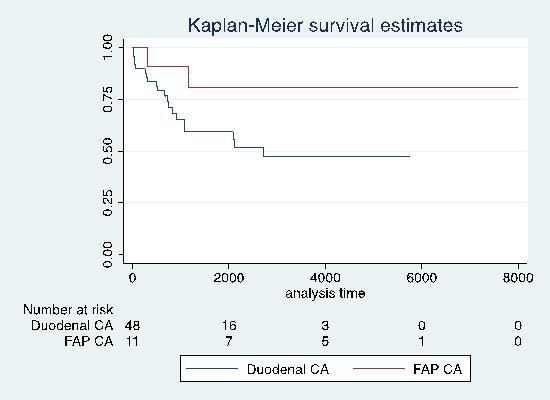
Comparing survival, FAP related duodenal cancer patients were noted to have a 70% lower unadjusted overall hazard of mortality compared to duodenal cancer patients, which approached statistical significance (Figure 1 Kaplan Meier survival curve; analyses time in days) (p 0.08).
CONCLUSIONS: FAP related duodenal cancer patients may have an improved survival compared to sporadic duodenal cancer. This may be related to an endoscopic surveillance program leading to earlier diagnosis and earlier stage as well as younger age at presentation. Consideration should be given to adjuvant therapy for all patients with new chemotherapeutic regimens to improve overall survival.
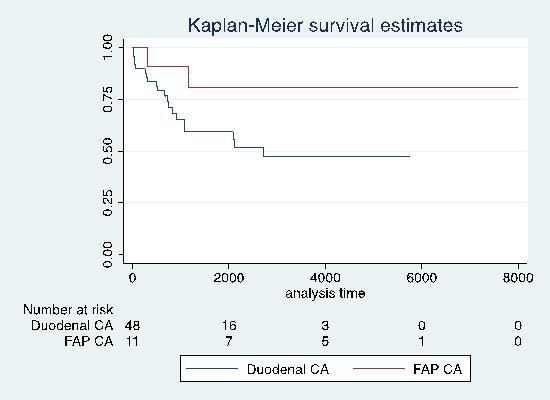
Figure 1: Kaplan Meier survival comparing FAP related duodenal cancer and sporadic duodenal cancer groups.
Back to 2017 Program and Abstracts
|