|
Back to 2017 Program and Abstracts
IS NEOADJUVANT THERAPY SUFFICIENT IN RESECTED PANCREATIC CANCER PATIENTS? A NATIONAL STUDY
Susanna W. de Geus*1, Gyulnara G. Kasumova1, Mariam F. Eskander1, Sing Chau Ng1, Tara S. Kent1, A. J. Moser1, Alexander L. Vahrmeijer2, Mark P. Callery1, Jennifer F. Tseng1
1Surgery, Beth Israel Deaconess Medical Center, Boston, MA; 2Surgery, Leiden University Medical Center, Leiden, Netherlands
Background: Adjuvant chemo(radio)therapy is considered standard of care in resected pancreatic cancer patients. However, despite increasing use of neoadjuvant treatment, the question of whether preoperatively treated, successfully resected patients should receive additional postoperative adjuvant treatment remains unanswered. We evaluated the impact of adjuvant therapy succeeding neoadjuvant treatment and pancreatectomy in pancreatic cancer patients in a large national study.
Methods: We used National Cancer Data Base (NCDB) 2006-2014 to identify resected, non-metastatic pancreatic adenocarcinoma patients who received preoperative chemotherapy +/- radiation followed by pancreatectomy. Patients that received only palliation were excluded. Patients expiring <6 months from diagnosis or time of surgery were excluded to control for immortality bias. Kaplan-Meier and multivariate Cox proportional hazard regression analyses were performed to compare survival between groups. Neoadjuvant treatment was defined as chemotherapy +/- radiation, and adjuvant treatment comprised of chemotherapy and/or radiation.
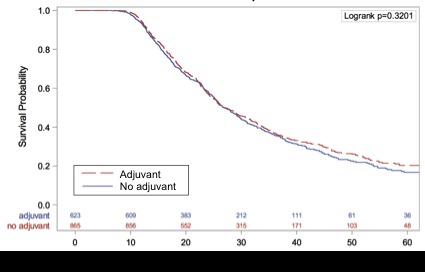
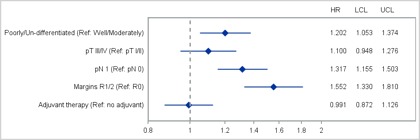
Results: In total, 1,488 patients were identified. 865 (58.1%) patients solely received neoadjuvant therapy followed by surgery and 623 (41.9%) received additional adjuvant therapy after preoperative treatment succeeded by surgery. There was no difference in unadjusted median overall survival between patients who did and did not receive additional adjuvant therapy (median survival, 27.1 months from diagnosis vs. 26.9 months respectively, p=0.320). On multivariate Cox modeling, receipt of additional adjuvant therapy was not predictive of survival (HR: 0.99; 95% CI: 0.87-1.13; p=0.89); however, poorly/undifferentiated grade (HR: 1.20; 95% CI: 1.05-1.37; p=0.007), positive nodal status (HR: 1.32; 95% CI: 1.16-1.50; p<0.0001), and positive resection margins (HR: 1.55; 95% CI: 1.33-1.81; p<0.0001) were predictors of mortality following neoadjuvant treatment. Even in these less favorable groups, postoperative adjuvant therapy was not significantly associated with favorable prognosis in patients with positive resection margins (p=0.532) or positive lymph nodes (p=0.481) following neoadjuvant therapy and surgery.
Conclusions: Postoperative adjuvant therapy has been definitively shown to improve survival for chemo-naïve, up-front surgery patients undergoing pancreatectomy for pancreatic adenocarcinoma. Our results using national data demonstrate a 27-month survival for patients undergoing neoadjuvant treatment / resection that is not impacted by additional postoperative adjuvant therapy. After receipt of preoperative chemo(radio)therapy and pancreatectomy, additional adjuvant therapy may not be required. These data warrant further prospective data collection and consideration for clinical trials.
Kaplan-Meier curve for all pancreatic cancer patients that received preoperative chemo(radio)therapy and pancreatectomy by receipt of adjuvant therapy.
Forest plot for multivariate Cox proportional hazard regression analysis in pancreatic cancer patients that received preoperative chemo(radio)therapy and pancreatectomy.
Back to 2017 Program and Abstracts
|