|
Back to 2017 Program and Abstracts
COMPARATIVE EFFECTIVENESS OF SURGICAL RESECTION VERSUS LIVER TRANSPLANTATION FOR HEPATOCELLULAR CARCINOMA: FACTORING IN THE WAIT-LIST DROP OFF RATE
Curtis J. Wray*, Mark J. Hobeika, Tien C. Ko, Lillian S. Kao
Surgery, University of Texas Medical School at Houston, Houston, TX
Introduction: Observational studies have demonstrated a survival advantage amongst hepatocellular carcinoma (HCC) patients treated with liver transplantation (LT) compared to liver resection (LR). However, it is unknown whether this survival advantage is due to selection bias as patients who experience tumor progression or death drop off the wait-list and are excluded from data analysis. Published reports of wait-list drop off approach 20%. The purpose of this study is to determine whether LT advantage still exists if wait-list drop off patients were factored into the survival model.
Methods: The National Cancer Data Base was queried for HCC cases from 1998-2014. Patients meeting Milan Criteria and treated with either LR or LT were included in the analysis. Exclusion criteria were unknown tumor size, vital status or surgery. Standard demographic and pathologic variables were used to create an inverse probability of treatment weighted propensity score and included in a Cox regression to estimate the survival difference between LR and LT. To account for LT wait-list drop off, simulated data was created from NCDB for patients meeting Milan Criteria, but who did not undergo LT or LR. To estimate the effect upon survival, simulated waitlist drop off rates of 5, 10, 15, 20 and 25% patient were included in sequential survival models. Assumptions included that no crossover occurred and that patients who dropped out did not receive other surgical intervention.
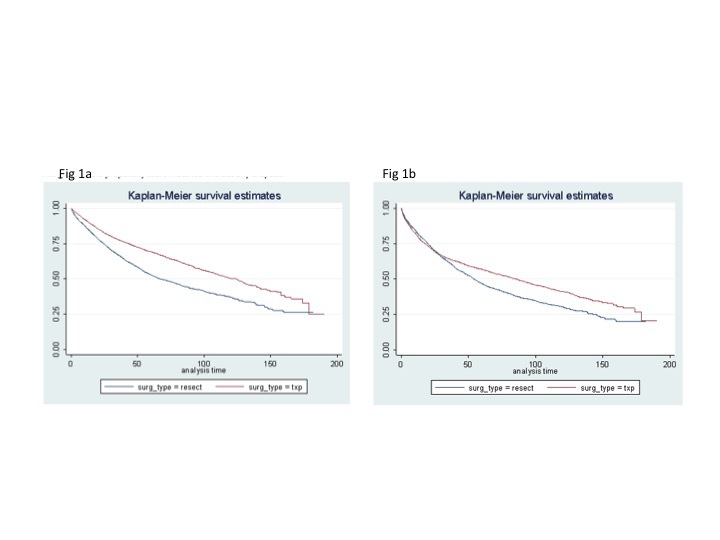
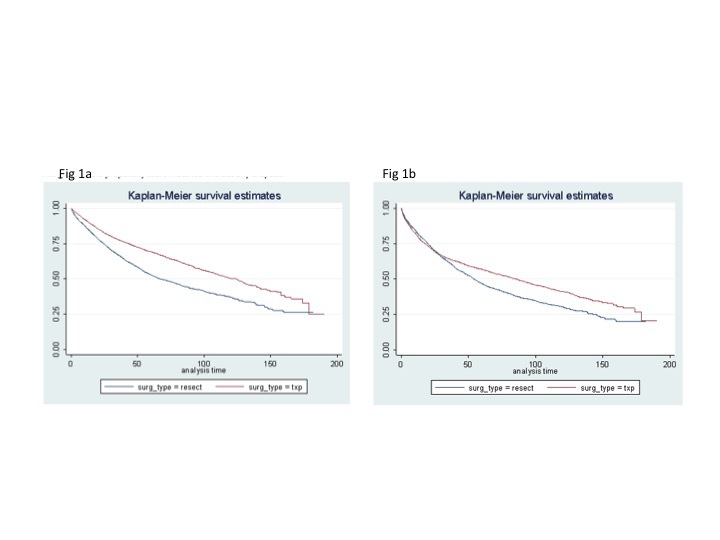
Results: 12,902 patients (n=7421 LT, n=5481 LR) met study criteria. There were differences between cohorts as a higher proportion of LT patients were male (78% vs. 69%), Caucasian (67% vs. 60%), privately insured (56% vs. 40%) and younger in age (57 years vs. 63 years)(P<0.05). Adjusting for these differences, at a drop off rate of 0%, there is a significant advantage for LT (HR 0.58, 95%CI:0.53-0.64)(Figure 1a). Once waitlist drop off is included in the model, diminished survival is observed as the HR increased: 5% (HR 0.70), 10% (HR 0.76), 15% (HR 0.84) and 20% (HR 0.88). At a 25% drop off rate, there is no significant difference between LT and LR (HR 0.92, 95%CI:0.85-1.01)(figure 1b).
Conclusions: We used a novel technique of incorporating simulated data into the survival analysis and have shown that transplantation provides an advantage over LR for HCC patients only at low wait-list drop off rates. This data suggests that transplant centers should focus efforts on keeping the drop off rate below 20%. An unbiased assessment of the comparative effectiveness of these two methods of treating HCC is critical to improving survival, especially in the era of uncertain changes in LT organ allocation policy.
Back to 2017 Program and Abstracts
|