|
Back to 2017 Program and Abstracts
STRATEGIES FOR SURGICAL REMEDIATION OF THE MULTI-FUNDOPLICATION FAILURE PATIENT
Michael Antiporda*, Chloe Jackson, C D. Smith, Mathew Thomas, Enrique F. Elli, Steven P. Bowers
General Surgery, Mayo Clinic Florida, Jacksonville, FL
Introduction:
Outcomes are not well studied in patients who undergo remediation for multi-fundoplication failure, that is, two-or-more prior failed fundoplication or hiatal operations. Re-operation must balance reflux control and restoration of the ability to eat with the challenge of reconstructing an anatomically distorted hiatus and GE junction. The purpose of this study is to present our experience with surgical remediation for multi-fundoplication failure and characterize an algorithm to reduce future operative intervention and remediate symptoms.
Methods:
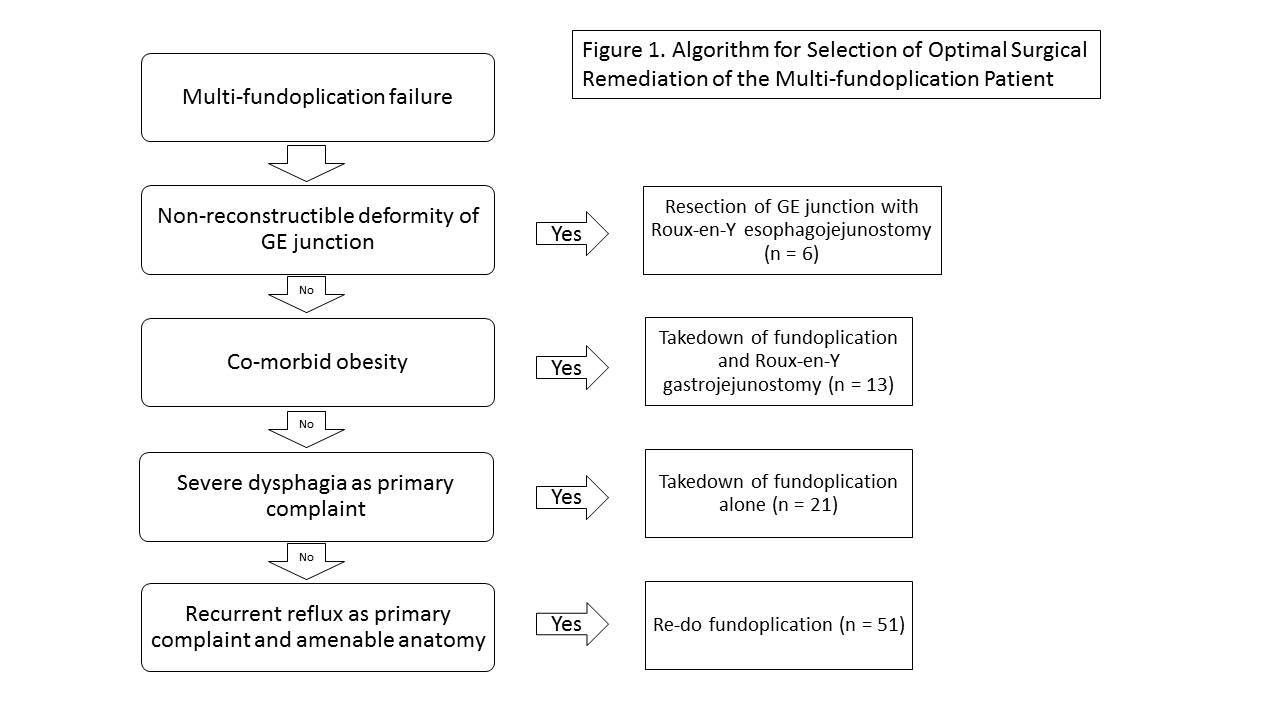
Medical records were retrospectively reviewed of 91 patients who underwent third time or more revisional fundoplication and/or hiatal hernia repair at a single institution from 2007 to 2016. Dysphagia was primary symptom in 51 patients (56%) and reflux symptoms were present in 46 patients (51%). The median number of prior operations was 2 with range up to 6. Anatomic failure consisted of slipped wrap in 26, wrap herniation in 22 cases, hiatal stenosis in 24, hiatal mesh complication in 8, gastroparesis in 3, and wrap dehiscence with recurrent reflux in 8. Operative approaches generally followed the algorithm (Figure 1) and consisted of hiatal hernia repair with: re-do fundoplication in 51 patients (56%), takedown of fundoplication alone in 21 (23%), Roux-en-Y gastrojejunostomy in 13 (14.3%), and GE junction resection with Roux-en-Y esophagojejunostomy in 6 (6.5%). Laparoscopic approach was successful in 81% of cases, laparotomy was necessary in 16%, and two-field thoracoabdominal approach in 3%.
Results:
Mean duration of operations was 217 minutes and median length of stay was 3 days. The complication rate was 11% with 6.6% of patients undergoing an unplanned early re-operation. There was one 30-day mortality due to necrotizing pneumonia. Patients were followed for mean 11 months, and recurrent fundoplication failure was detected in 13% of patients. Late reoperation was performed in 5.5% for recurrent symptomatic failure. Recurrent reflux symptomatology resolved in 93.4% of cases post-revision. Dysphagia resolved in 84% of cases. There were no significant differences in outcomes with regard to number of prior operations, operative approach, BMI, or age.
Conclusion:
There is no single best approach to remediation in the multi-fundoplication failure patient and redo fundoplication is appropriate in over half of patients. Reoperation for multi-fundoplication failure can be performed via minimally invasive approach and with excellent remediation of symptoms, low morbidity and low late recurrence rates.
Back to 2017 Program and Abstracts
|

