|
 |
Back to 2017 Program and Abstracts
ENDOSCOPIC GASTROJEJUNAL REVISION RESULTS IN MORE WEIGHT LOSS THAN MEDICAL MANAGEMENT ALONE FOR WEIGHT REGAIN AFTER GASTRIC BYPASS
Herbert M. Hedberg*1,2, Alexander Trenk2, Eliza Conaty2, John G. Linn2,1, JoAnn Carbray2, Michael Ujiki2,1
1Surgery, University of Chicago, Chicago, IL; 2Surgery, NorthShore University HealthSystems, Evanston, IL
Background
Weight regain following Roux-en-Y Gastric Bypass (RYGB) is common, affecting up to 30% of individuals. Regain is often due to dilation of the gastrojejunostomy, resulting in decreased restriction and postprandial satiety. Recent development of endoscopic suturing devices has allowed Endoscopic GastroJejunostomy Revision (EGJR) as a safe alternative to revisional surgery, which carries increased risk compared to initial operation. EGJR results in weight loss, but existing studies do not compare weight over time to a similar cohort that did not receive revision.
Methods
Patients who received EGJR between the years 2012 and 2016 were identified in a prospectively collected database for retrospective analysis. A control cohort was retrospectively compiled consisting of patients who were seen in consultation to address weight regain after RYGB, were deemed appropriate candidates for EGJR, but did not receive the intervention. Both groups received dietary consultation and psychological testing. Maximum pre RYGB weight, post RYGB nadir, weight at consultation for revision, and post consultation weight at six months, one year and two years after consultation was collected. To standardize weights for comparison, ideal body weight was found using the J. D. Robinson Formula and %Excess Body Weight Loss (%EBWL) was calculated for each timepoint using maximum pre RYGB weight as a reference. Student’s t-test was used to compare %EBWL at each timepoint.
Results
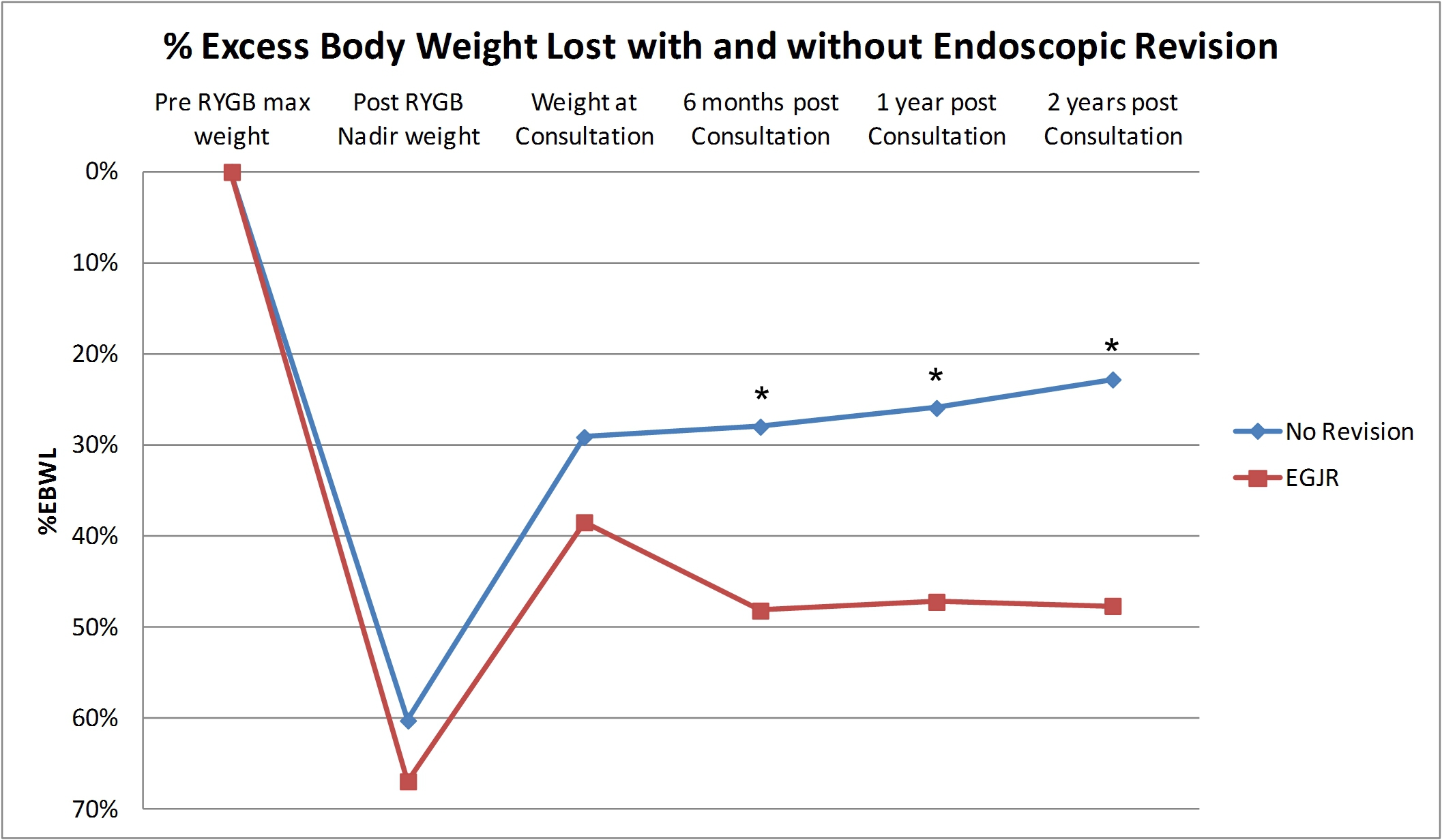
At time of consultation, there were 40 patients in the EGJR group and 17 in the no revision group. The EGJR group was 92.5% female and the no revision group 82.3% female. There was no statistical difference between time from RYGB to consultation (9.4±3.2 years vs 7.8±3.4 years). Prevalence of hypertension, sleep apnea, diabetes, and hyperlipidemia between the groups was similar. Among the six time points, %EBWL was significantly higher in the endoscopic revision group at six months, one year, and two years (see Chart 1). Comorbidities at one year were available for 14 individuals in the EGJR group and 8 in the no revision group. One individual in the EGJR group was no longer on medication for hyperlipidemia, and another no longer on medication for hypertension, while there were no resolved comorbidities in the revision group.
Conclusion
EGJR for weight gain after RYGB is a safe alternative to revisional surgery. In this study, individuals who received EGJR were compared to a cohort of similar patients deemed appropriate for EGJR, yet did not have the procedure. The groups had similar %EBWL at their nadir weight after RYGB and at the time of consultation concerning weight regain. After the study group received EGJR, %EBWL diverged. The EGJR group approached and maintained 50% EBWL over a two year period, while those without revision showed a trend toward continued weight gain.
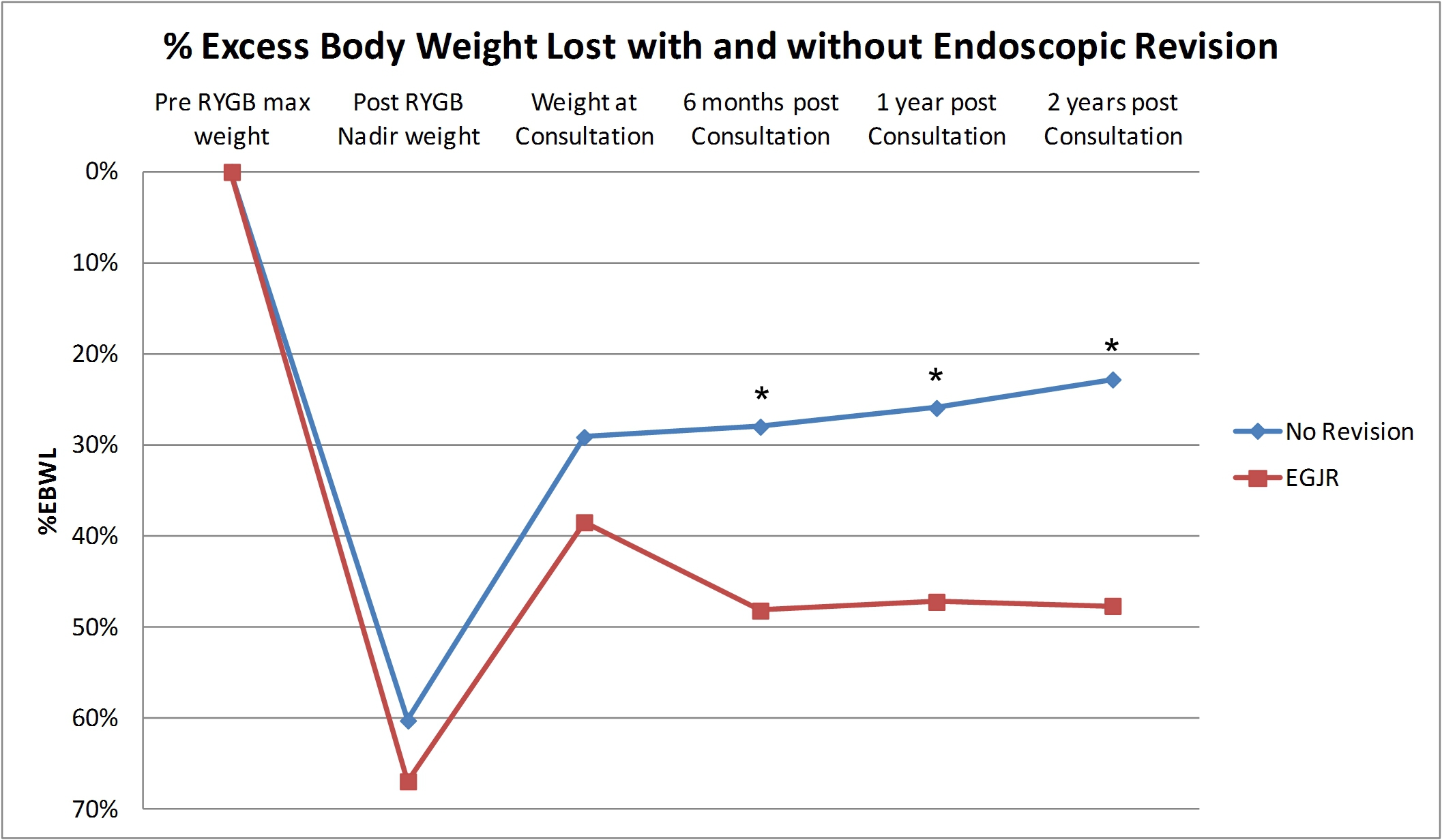
Figure 1: Visual representation of %Excess Body Weight Loss (%EBWL) after RYGB over time, with and without endoscopic revision. * = significant divergence between groups.
Back to 2017 Program and Abstracts
|