|
 |
Back to 2017 Program and Abstracts
SERIAL ENDOSCOPIC EVALUATION OF ESOPHAGEAL DISEASE IN A CANCER MODEL: A PARADIGM SHIFT FOR ESOPHAGEAL ADENOCARCINOMA (EAC) DRUG DISCOVERY AND DEVELOPMENT
Ashten N. Omstead*1, David A. Guel1, Daisuke Matsui1, Juliann E. Kosovec1, Samantha Martin1, Emily J. Smith1, Jenna Kolano1, Patrick Campbell1, Haley Raphael1, Fahim Habib1, Kevi Christopher1, Christopher Lai1, Matthew A. Smith2, Ronan J. Kelly3, Ali H. Zaidi1, Blair A. Jobe1
1Esophageal and Lung Institute, Allegheny Health Network, Pittsburgh, PA, United States Minor Outlying Islands; 2Department of Pathology and Laboratory Medicine, Allegheny Health Network, Jefferson Hills, PA; 3Medical Oncology, Johns Hopkins Sidney Kimmel Comprehensive Cancer Center, Baltimore, MD
Introduction:
EAC is rising in incidence and is associated with poor overall survival, thereby establishing the need to develop and improve available treatment options by utilizing disease-representative cancer models. The modified Levrat model of surgically induced gastroduodenoesophageal reflux (GDER) has been shown to effectively recapitulate the physiological and molecular progression of EAC, as seen in humans. However, the use of the model for studying in vivo disease progression and therapeutic efficacy of novel agents is fairly limited due to primary reliance on postmortem histology as a screening tool. The objective of the current study was to establish small animal endoscopy with biopsy as an in vivo approach to diagnose and monitor EAC in live animals.
Methods:
GDER was induced in 21 Sprague-Dawley rats by the modified Levrat surgery. Between 17 and 38 weeks post-surgery, all animals underwent endoscopy with biopsies, using a rigid Karl Storz endoscope (diameter 1.9/2.1 mm) with 1 mm pinch biopsy forceps. Post-endoscopy, all animals were immediately sacrificed for final histology which served as the gold standard for inter-group comparisons with visual endoscopy and biopsy. The endoscopic videos and biopsies were read by four blinded esophageal endoscopists and a pathologist, respectively. Accuracy, sensitivity, specificity and Kappa coefficient were used for intergroup comparisons.
Results:
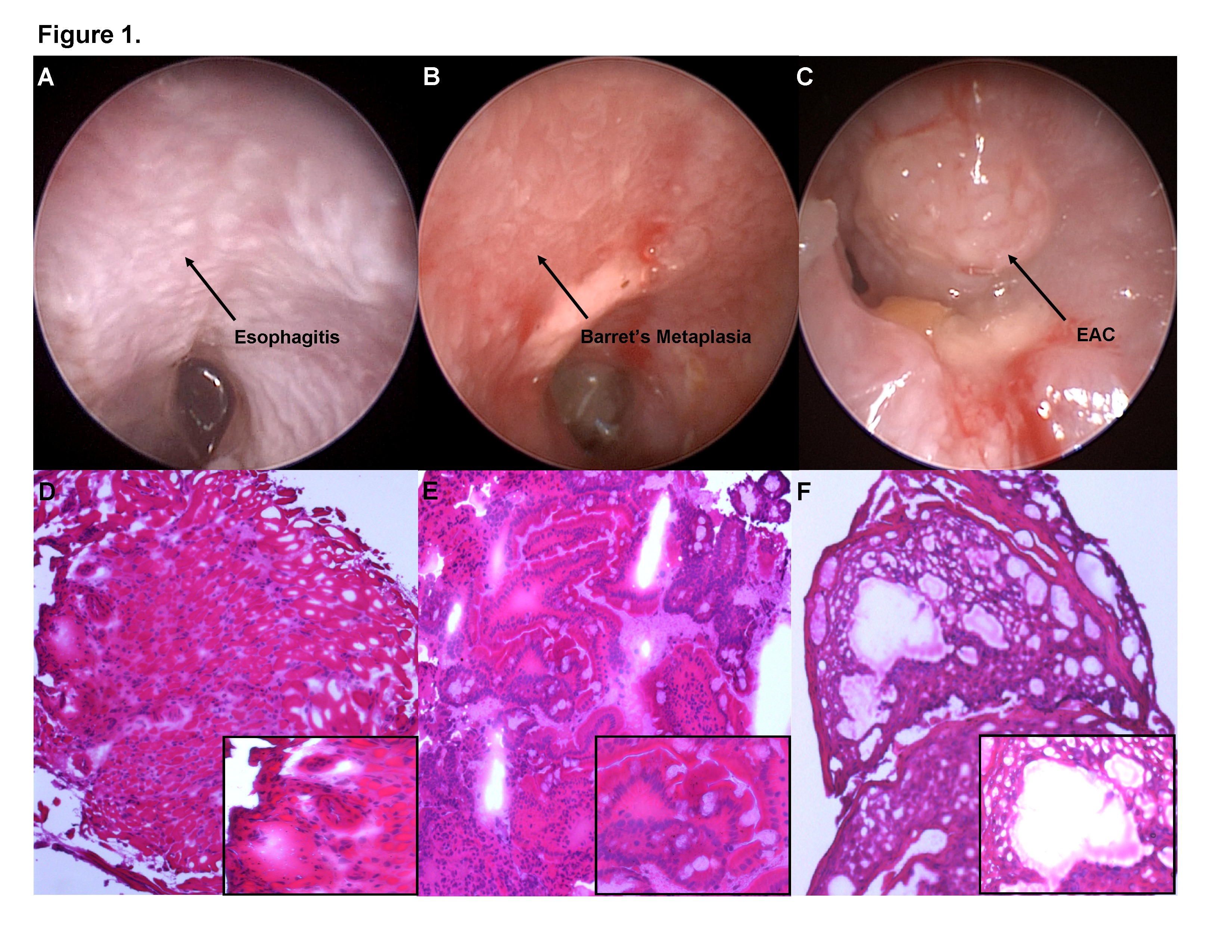
The overall accuracy of the visual endoscopy to correctly identify esophageal disease was 86%, with a sensitivity and specificity of 92% and 100%, respectively - Table 1. The Kappa coefficient for the comparison was 0.904. The classification accuracy of Barrett’s (BE) with dysplasia only was 100%, and the classification accuracy of EAC only was 75% - Figure 1. The overall accuracy of the use of endoscopic biopsy to correctly identify esophageal disease was 59%, with a sensitivity and specificity of 53% and 100%, respectively - Table 1. The Kappa coefficient for the comparison was 0.523. The percentage agreement between biopsies and post-mortem histology for BE with dysplasia only was 44% and for EAC only was 75% - Figure 1. Interestingly, for esophageal tumors >4 mm, the percentage agreement of endoscopic biopsy with post-mortem histology increased to 78%, with sensitivity and specificity of 75% and 100%, respectively. Additionally, the pathologist identified 58% biopsy specimens as samples with artifact / poor orientation, inadequate tissue depth or low confidence histology.
Conclusions:
Visual assessment with endoscopy can reliably assess disease progression in the modified Levrat model. The ability to reliably detect disease and simultaneously obtain biopsies for downstream molecular correlates establishes the model as an important tool to evaluate and determine efficacy of novel agents for the treatment of esophageal cancer.
Table 1.
| | BE with Dysplasia Endoscopy | EAC Endoscopy | BE with Dysplasia Biopsy | EAC Biopsy | | True Positive | 9 | 11 | 4 | 9 | | False Positive | 0 | 0 | 0 | 0 | | False Negative | 0 | 1 | 5 | 3 | | True Negative | 12 | 9 | 12 | 9 |
Table 1. Total of correct and incorrect esophageal disease classifications for endoscopy and biopsy histology, used to calculate sensitivity and specificity. 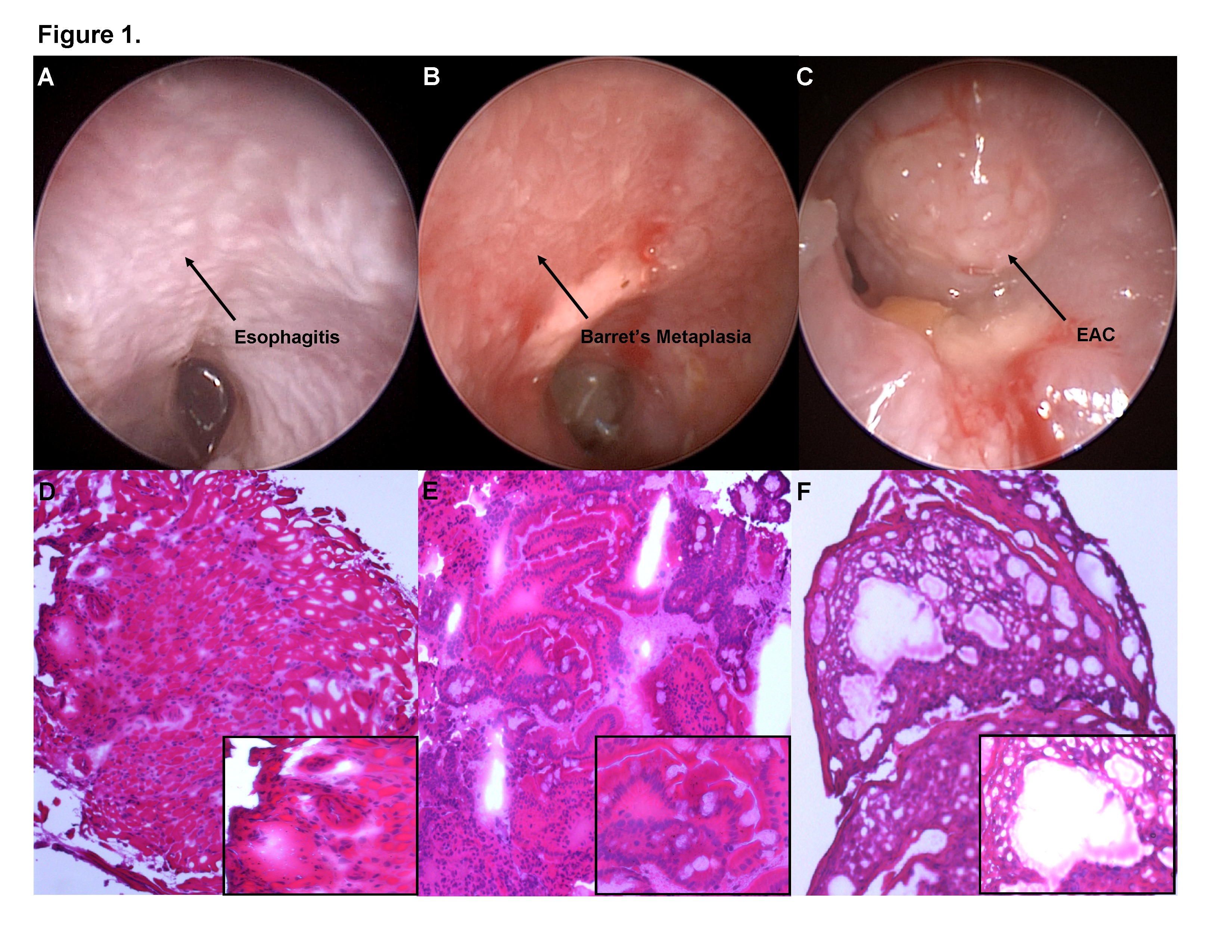 Figure 1. Figure 1. Endoscopic image and corresponding biopsy histology, at 10X and 40X, for each esophageal disease stage; A. Esophagitis, B. Barrett’s Esophagus, C. Esophageal Adenocarcinoma.
Back to 2017 Program and Abstracts
|