|
Back to 2017 Program and Abstracts
RURAL-URBAN AND REGIONAL DIFFERENCES IN RECEIPT OF ESOPHAGECTOMY FOR EARLY-STAGE ESOPHAGUS CANCER
Emily C. Sturm*, Whitney Zahnd, Erin Mackinney, John D. Mellinger, Sabha Ganai
Surgery, Southern Illinois University School of Medicine, Springfield, IL
Introduction
Recent studies have shown superior in-hospital outcomes for esophagectomy performed at high-volume centers, subsequently creating momentum toward centralization of esophageal cancer care. However, the impact of rural location on overall survival of esophageal cancer has not been studied. We hypothesize that there will be regional differences in surgical management of esophageal cancer and that rural patients will have a decreased survival because of access disparities.
Methods
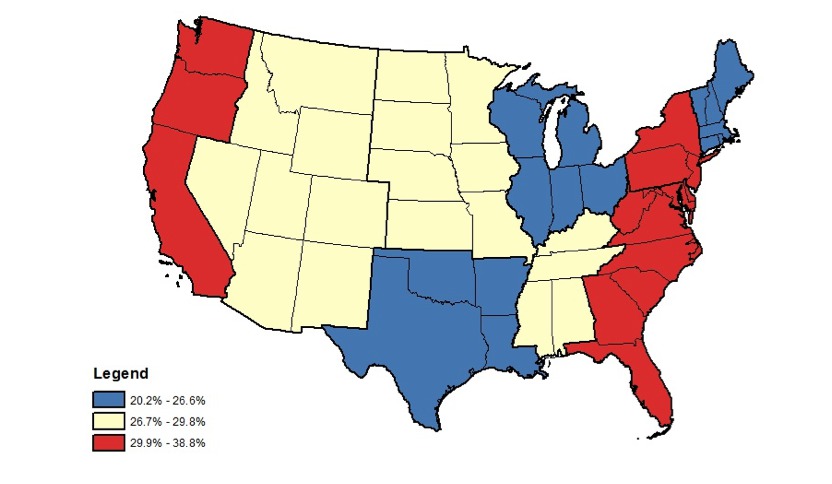
The National Cancer Database was queried for cT1 or cT2 esophageal cancer cases diagnosed between 1998 and 2012 with a valid rural-urban designation (n=21,981). The proportions of patients who had surgical resection by rural-urban status and region were compared based on demographic and clinical characteristics. Rural-urban status was determined by the United States Department of Agriculture’s Rural Urban Continuum Codes, which categorize counties by population size and proximity to a metro area. Chi-square test was performed for independence to compare the proportion of patients who had surgical resection by rural urban status and region, and choropleth maps were developed to show tertiles of resection by region. Kaplan Meier curves were constructed to assess survival by rural urban status. Adjusted Cox Regression was performed to determine rural-urban differences in survival accounting for demographic, treatment, geographic, pathologic stage, and facility characteristics.
Results
Early stage clinical T1-T2 esophageal cancer patients varied by demographic, geographic, and facility characteristics. A greater proportion of rural patients underwent esophagectomy (29%) compared to urban patients (27%) (p=0.006). When comparing specific geographic regions, more patients underwent esophagectomy among rural patients compared to urban patients in the Middle Atlantic (38% vs. 28%, p=0.0002) and Pacific (39% vs. 29%, p=0.005) regions. There was no statistically significant difference in any other regions. Median driving distance was longer for rural patients (41 miles) compared to urban patients (8 miles). In adjusted analysis including controlling for facility type, pathologic stage, and receipt of neoadjuvant therapy, there was no statistically significant difference between rural and urban patient survival.
Conclusion
As we hypothesized, there were regional differences in surgical management of esophageal cancer, but in the Middle Atlantic and Pacific regions of the United States, rural patients were actually more likely to undergo esophagectomy compared to urban patients. Contrary to our hypothesis, however, despite historic data showing increased in-hospital mortality at low-volume centers, there was no statistically significant difference in overall survival between rural and urban patients who received esophagectomy. Overall esophagectomy rates remain low nationwide.
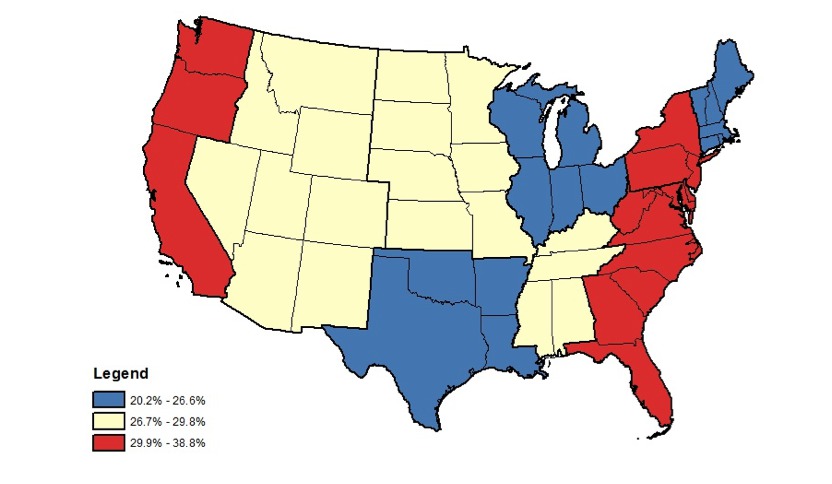
Figure: Regional Differences in Esophagectomy Rates for Rural Patients, Tertiles
Back to 2017 Program and Abstracts
|