|
Back to 2017 Program and Abstracts
TREATMENT VARIABILITY FOR LOCALLY ADVANCED ESOPHAGEAL CANCER IN THE UNITED STATES AND ITS EFFECT ON LONG-TERM OUTCOMES
Arianna Barbetta*1, Anne O. Lidor2, Renee L. Gennarelli3, Elena Elkin3, Matthew Bott1, James Isbell1, Manjit S. Bains1, David R. Jones1, Daniela Molena1
1Department of Thoracic Surgery, Memorial Sloan Kettering Cancer Center, New York, NY; 2Department of Surgery, University of Wisconsin, Madison, WI; 3Department of Epidemiology & Biostatistics, Memorial Sloan Kettering Cancer Center, New York, NY
Objectives: National guidelines for the treatment of locally advanced esophageal cancer have been developed to standardize care and improve results of this deadly disease. The goal of our study was to evaluate how patients (‚Č•65 year-old) with esophageal cancer are treated in the United States and how different treatment strategies affect long-term outcomes.
Materials and Methods: We used the Surveillance, Epidemiology and End Results (SEER)-Medicare database to identify patients diagnosed with locally advanced esophageal from 2004-2011 who had treatment with curative intent. Patients with cervical esophageal cancer were excluded. The study cohort was limited to patients who had surgery Ī adjuvant therapy, definitive radiation, definitive chemoradiation, or induction therapy (chemotherapy and/or radiation) and surgery within 180 days of diagnosis. Multinomial logistic regression was used to examine associations between treatment and demographic factors controlling for clinical characteristics. Overall survival among propensity score-matched treatment cohorts was compared using Kaplan-Meier estimates.
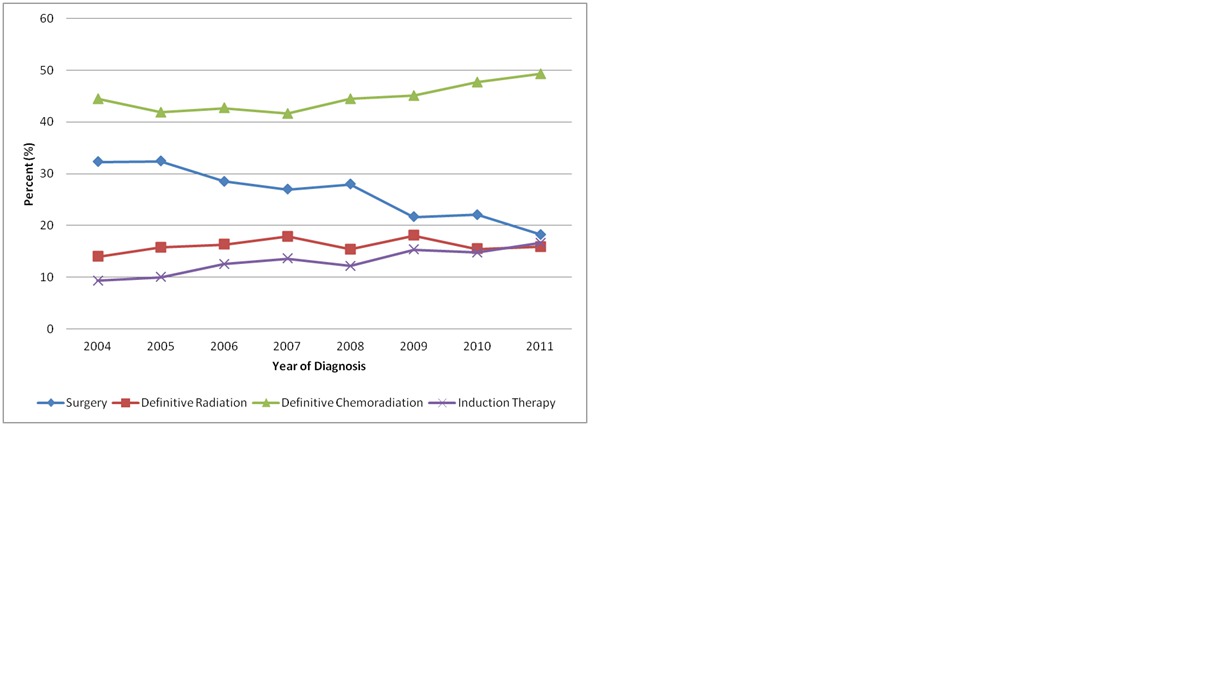
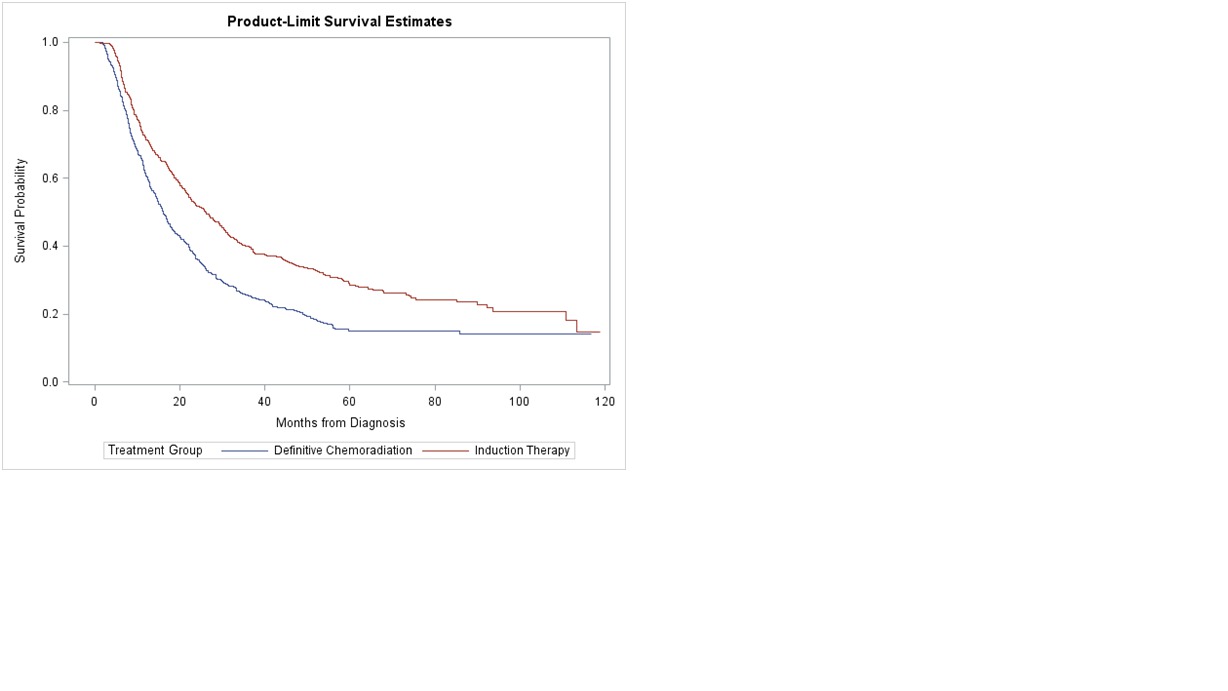
Results: We identified 4,478 patients treated for locally advanced esophageal cancer. Adenocarcinoma was the most common histology (73%). The majority (45%) were treated with definitive chemoradiation, surgery (26%), radiation (16%), and induction therapy followed by surgery (13%). The use of multimodality therapy among those being treated with curative intent increased during the study period, while surgery decreased (Fig. 1). The type of treatment received was associated with demographic factors after controlling for clinical characteristics. After propensity score matching, induction therapy followed by surgery had a significantly higher 5-year overall survival compared to definitive chemoradiation (28% vs. 15%, p<0.01) (Fig. 2). Alternatively, there was no difference in 5-year overall survival between patients treated with surgery and those treated with induction therapy followed by surgery (32% vs. 31%, p=0.3).
Conclusions: In our study, very few elderly patients with locally advanced esophageal cancer in the United States were treated according to national guidelines. Surgical resection is likely the most important aspect of treatment and provides the best chance for improved survival. Despite a prevailing nihilistic view regarding outcomes for this dreaded disease, surgery should be considered for all patients with acceptable operative risks.
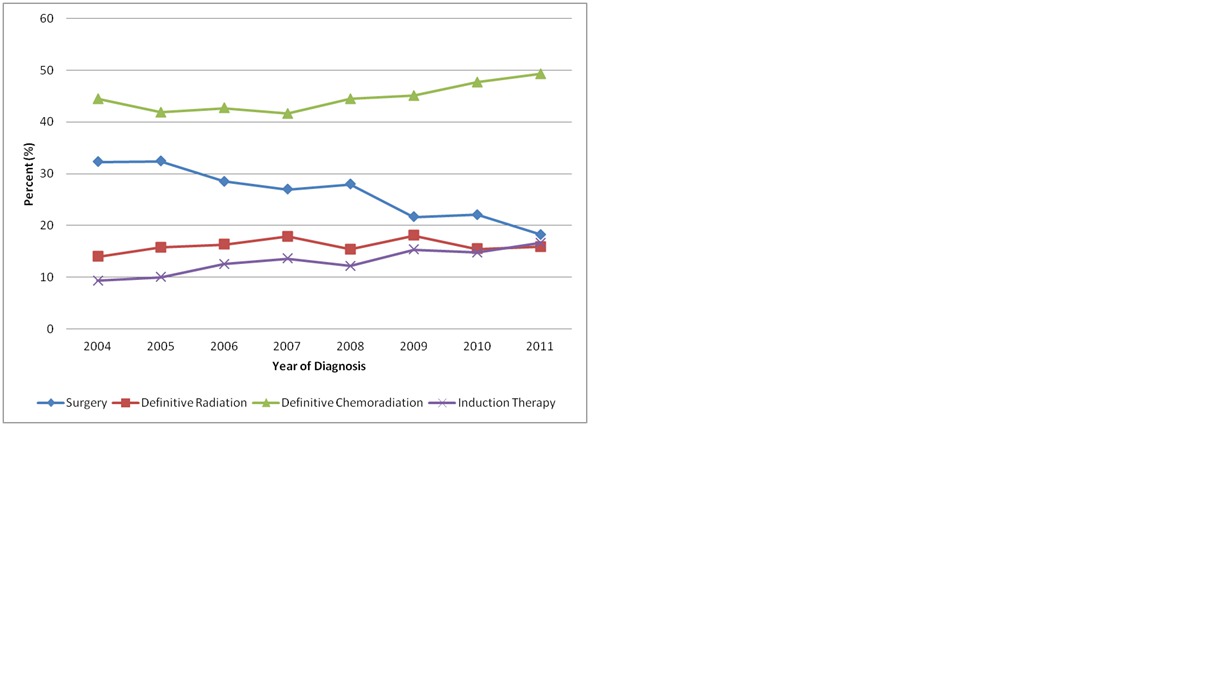
Fig. 1. Proportion of cohort treated by curative intent treatment group over time
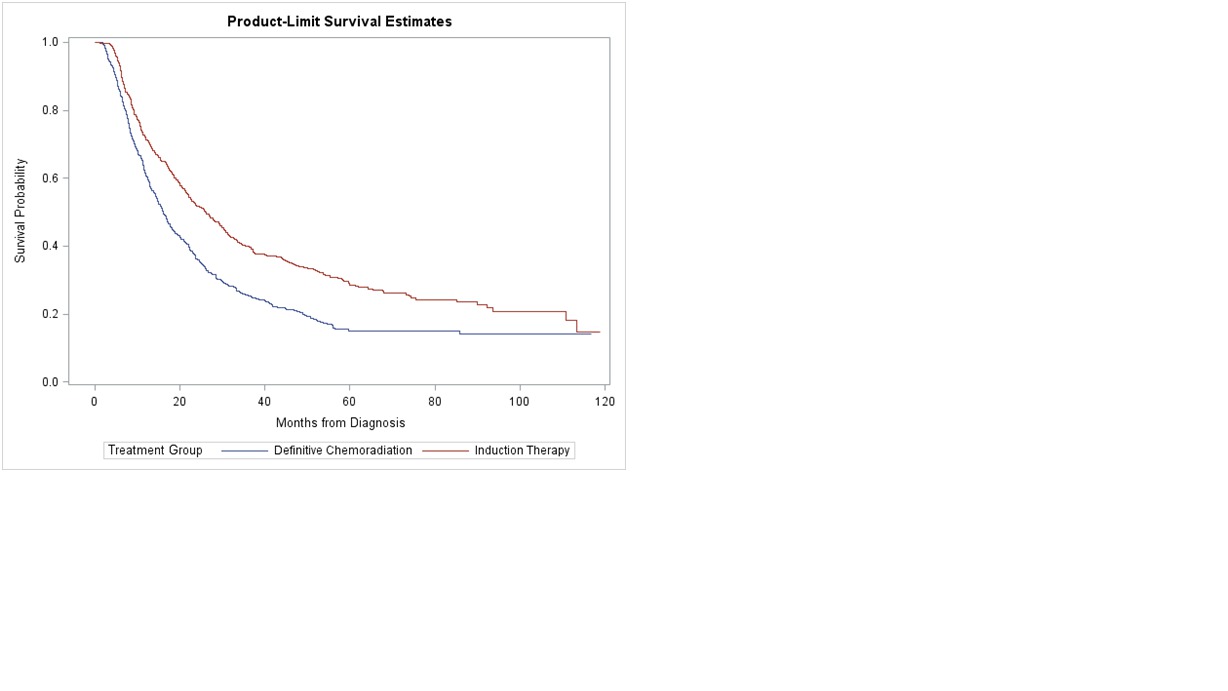
Fig. 2 Survival: Definitive Chemoradiation vs. Induction Therapy Followed by Surgery
Back to 2017 Program and Abstracts
|