|
Back to 2017 Program and Abstracts
GERD AND HIATAL HERNIA: PRESENCE AND SIZE INFUENCE THE CLINICAL PRESENTATION, THE ESOPHAGEAL FUNCTION AND REFLUX PROFILE
Francisco Schlottmann*1, Ciro Andolfi2, Fernando A. M. Herbella3, Marco G. Patti1
1Surgery, University of North Carolina, Chapel Hill, NC; 2University of Chicago, Chicago, IL; 3Surgery, Federal University of Sao Paulo, Sao Paulo, Sao Paulo, Brazil
Background: A hiatal hernia (HH) is a frequent finding in patients with GERD. Its presence alters the anatomic relationship between the lower esophageal sphincter (LES) and the diaphragmatic crus, erasing their synergistic action and therefore eliminating a key component of the antireflux mechanism.
Aim: The aim of this study was to determine how the presence and size of a HH affect the esophageal function, the reflux profile and the degree of mucosal injury.
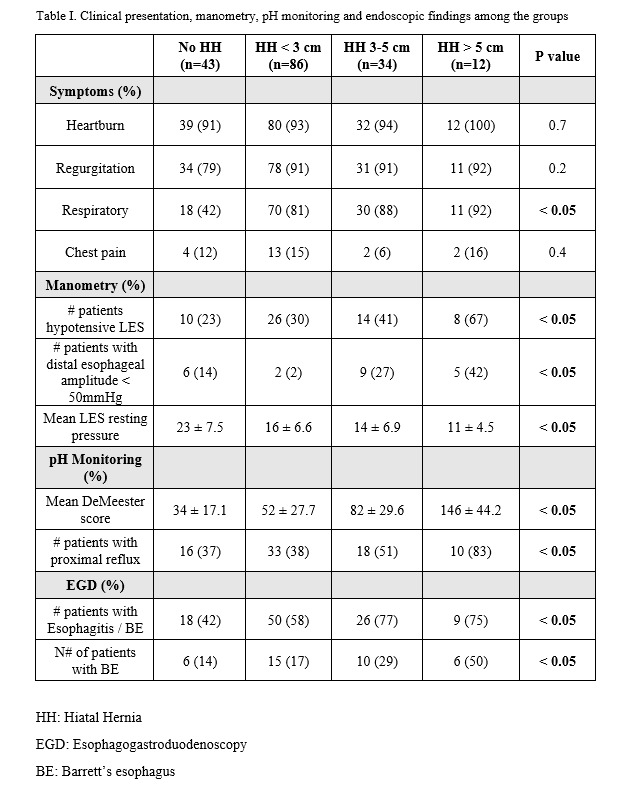
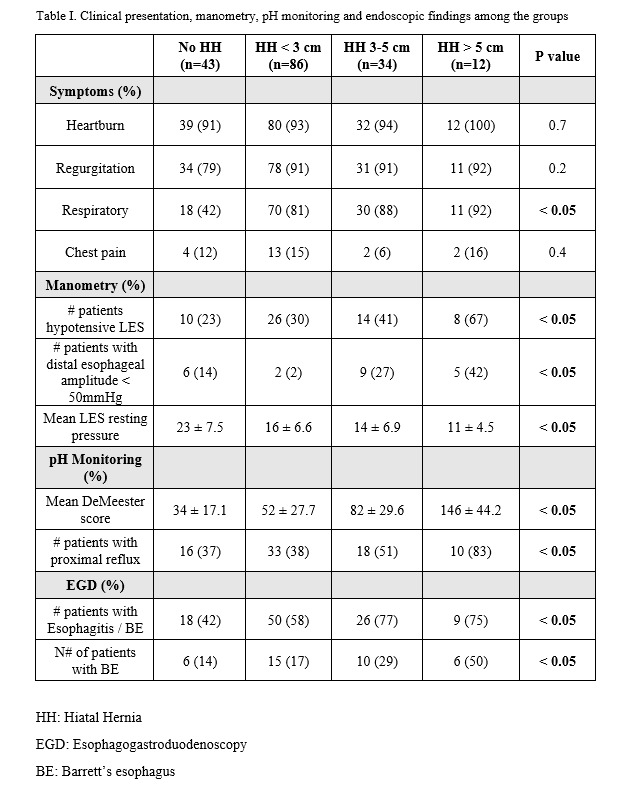
Patients and Methods: A consecutive series of patients with GERD diagnosed by 24-hour pH monitoring were included. Based on the presence and size of HH on barium swallow, patients were divided into the following groups: no HH, HH < 3cm, HH 3-5 cm and HH > 5 cm. Clinical presentation, esophageal manometry, pH monitoring and endoscopy findings were analyzed and compared between the groups.
Results: A total of 175 patients were included: 43 with no HH, 86 with HH < 3cm, 34 with HH 3-5 cm, and 12 with HH > 5 cm. Esophageal manometry showed that the increasing size of the HH was associated with decreasing pressure of the LES and weaker peristalsis. Ambulatory pH monitoring showed that patients with larger HH were exposed to more refluxed acid, in both the distal and proximal esophagus. These patients had more frequent episodes of coughing and wheezing associated with episodes of reflux. Endoscopy showed that patients with larger HH had more severe esophagitis. Fifty percent of patients with HH > 5.0 cm had Barrett’s esophagus (Table I).
Conclusions: In patients with proven GERD, presence and size of HH affect the clinical presentation, the manometric and reflux profile, and the degree of mucosal injury. These findings should guide gastroenterologists and surgeons in choosing the appropriate therapy to restore the competence of the gastroesophageal junction.
Back to 2017 Program and Abstracts
|