|
Back to 2017 Program and Abstracts
EFFECT OF ANTI-REFLUX SURGERY (ARS) ON SYMPTOM RESOLUTION AND QUALITY OF LIFE (QOL) IN PATIENTS WITH LARYNGOPHARYNGEAL REFLUX (LPR) WHO FAIL MEDICAL THERAPY
Fahim Habib*, Ali H. Zaidi, Yoshihiro Komatsu, Emily Lloyd, Samantha Martin, Emily J. Smith, Blair Jobe, Toshitaka Hoppo
Esophageal and Lung Institute, Allegheny Health Network, Pittsburg, PA
Background: Surgical outcomes in patients with LPR remain largely unknown. Prior studies on the impact of ARS on LPR have traditionally combined the entire constellation of symptoms (cough, globus, hoarseness, throat clearing, etc.) into one group limiting our understanding of symptom-specific response rates. We hypothesized that in appropriately selected patients, ARS will result in significant symptom resolution, thereby improving QOL.
Methods: Patients undergoing ARS for symptoms of LPR who had completed the Reflux Symptom Index (RSI) and Gastroesophageal Reflux Disease Health Related Quality of Life (GERD-HRQL) questionnaires before and after surgery were included. Selection for surgery was based on demonstration of abnormal proximal exposure (APE) using a specialized multichannel impedance catheter (HMII). APE was defined based on normative data previously established by our group. All patients had persistent symptoms despite aggressive medical management. A positive DeMeester score (DMS) was not required in the decision to pursue ARS. Outcome measures included: change in RSI and GERD-HRQL scores following ARS and resolution of specific symptoms of LPR. Comparisons utilized a paired Student’s t-test.
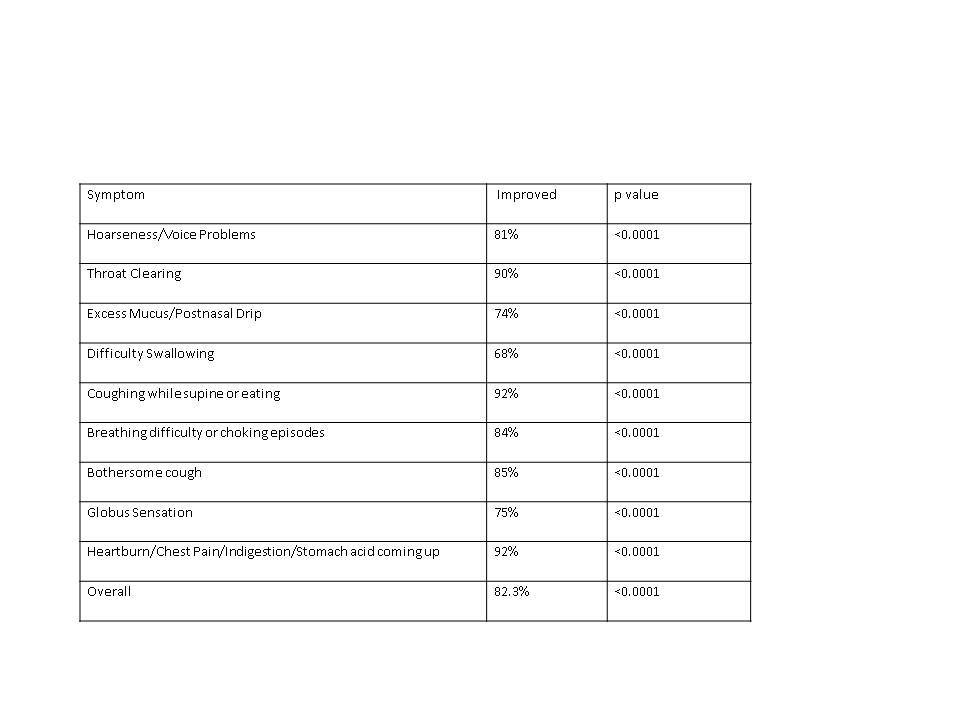
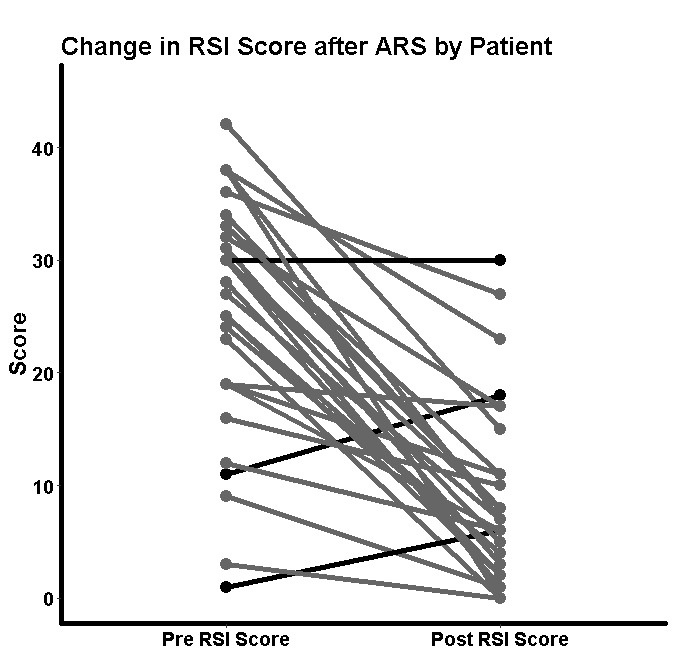
Results: Of 31 patients who met study criteria, 24 (77%) were female. Mean follow-up was 12 months. Overall, the primary, secondary, and tertiary presenting symptoms were cough (77%), hoarseness (65%) and heartburn (45%), respectively. Isolated LPR symptoms (absence of typical symptoms) were present in 11 of 31 (36%) combined LPR and typical symptoms were present in 20 of 31 (65%); cough was the primary presenting symptom in 91% of isolated and 50% of combined symptomatic patients in these two groups, respectively. DMS was negative in 10 (32%) patients. Twenty patients (65%) had reflux to the level of the hypopharynx, 8 (26%) into the proximal esophagus immediately distal to the upper esophageal sphincter, and 3 (10%) had reflux limited to the distal esophagus. Twenty-five underwent fundoplication and 6 had magnetic sphincter augmentation. Overall, the GERD-HRQL decreased from a mean of 13.84 to 2.97 (p<0.0001) and the RSI decreased from 25.16 to 8.68 (p<0.0001). An improvement in GERD-HRQL was seen in 27 of 31 (87%) and 28 of 31 (90%) had an improvement in the RSI [Figure 1]. All LPR symptoms improved but Cough and throat clearing were most responsive to ARS [Table 1]. Seventy-seven percent of patients were satisfied with the outcome of surgery. There was no difference in postoperative outcome between DMS+ and DMS- patients or those with isolated LPR symptoms vs. those with combined LPR and typical symptoms.
Conclusions: In patients with LPR symptoms and abnormal proximal exposure as defined by specialized HMII, ARS results in significant symptom improvement and QOL that is independent of preoperative DMS or the presence of typical symptoms.
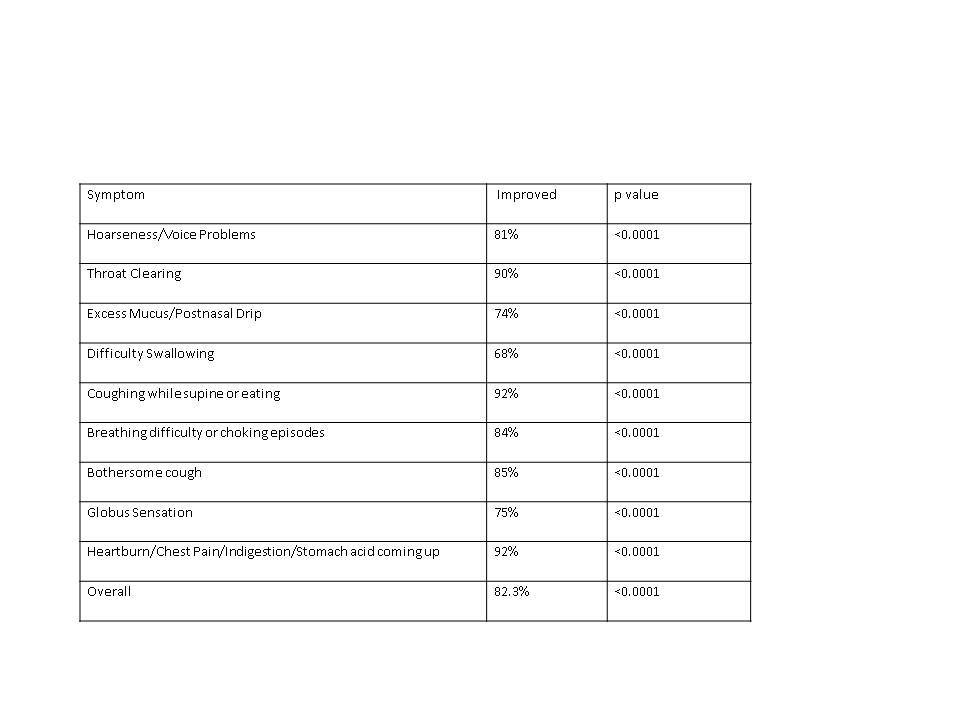
Table 1: Degree of Improvement of Individual Symptoms following Anti-reflux Surgery for Laryngopharryngeal Reflux
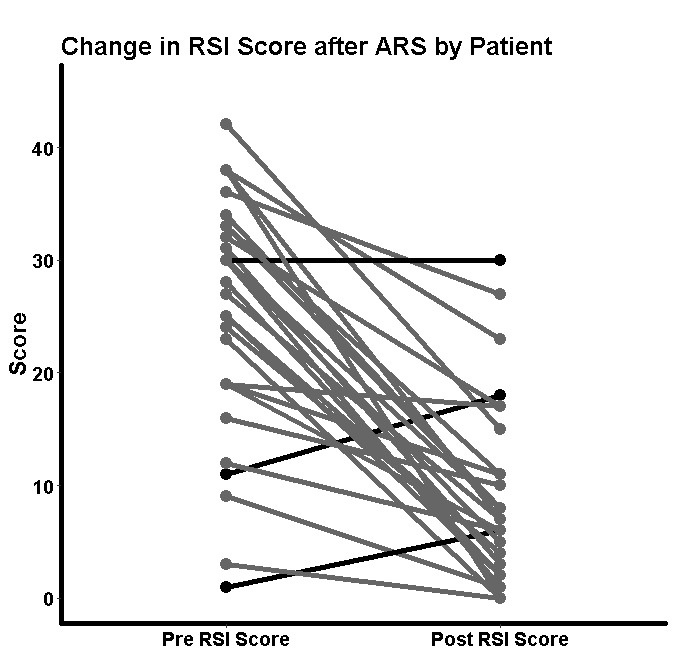
Figure 1: Change in RSI following anti-reflux surgery in patients with laryngopharyngeal reflux who failed medical therapy
Back to 2017 Program and Abstracts
|