|
Back to 2017 Program and Abstracts
PILOT STUDY OF A NOVEL MOBILE HEALTH APPLICATION TO TRACK PATIENTS AFTER GI SURGERY
Matthew Symer*, Jonathan S. Abelson, Bridget McClure, Heather Yeo
Surgery, NYP-Weill Cornell Medical Center, New York, NY
Introduction: The majority of readmissions after surgery are thought to be preventable and are commonly due to dehydration, ileus, malnutrition, and infectious complications. Smartphone-based mobile health technology has the potential to identify nascent complications before they require readmission.
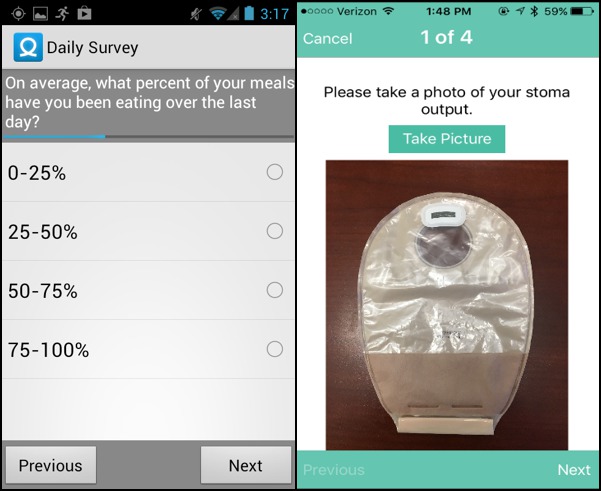
Methods: We performed a pilot study to prospectively evaluate the feasibility of a new mobile health application (mHEALS). mHEALS was developed based on a literature review of readmission and conversations with surgeons, nurses, and enterostomal nurses about parameters for monitoring patients postoperatively. The application had both active and passive components, including a short daily survey tailored to the patient's surgery type and presence or absence of an ostomy. Patients reported their average pain, were prompted to send photographs of their wounds, and reminded to stay hydrated. Activity data (sleep, heart rate, and step-count) were uploaded from a FitBit device. Abnormal or concerning patient responses triggered alerts to clinician investigators for further evaluation and informed patients to call their physician. Eligible patients were adults undergoing laparoscopic or open colorectal surgery. Patients were followed postoperatively for 30 days and their compliance with app use was tracked. Qualitative feedback was collected at the end of the trial.
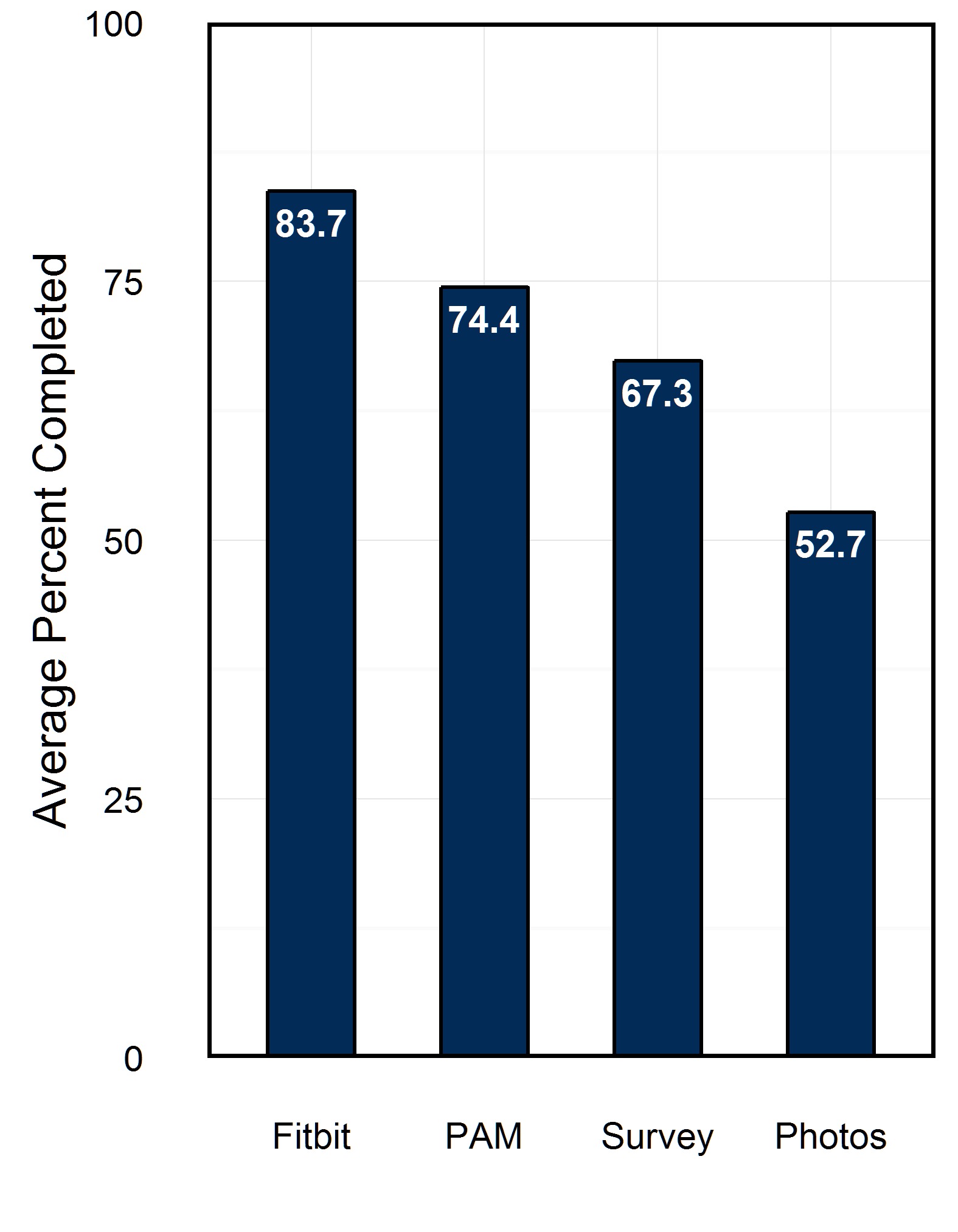
Results: 27 patients participated in the study and had a mean age of 50.8yo (range 21-75yo). Most were female (63%), and white (55.6%). 6(22%) had an ostomy as part of their surgery and 15(55.6%) used an iPhone. During the 30-day postoperative period 75% of patients completed at least 60% of the available survey tasks, meeting our apriori definition of feasibility (≥75%). Patients generated an average of 1.2 alerts during the study. Only one patient was readmitted in the cohort. The patient was readmitted for gastroenteritis and generated 7 alerts prior to re-admission. Average pain on post-operative days 1, 5, and 10 was rated 4.2, 5.1, and 3.8 respectively (out of 10). Patients participated most in collecting FitBit data (83.7% of days) and completing a single-item Photo Affective Meter (PAM), but had more difficulty regularly uploading photographs (52.7% completed of all possible photos). After study completion 91.7% of patients found the application easy to use and 91.3% would recommend the application to a friend.
Conclusion: It is feasible to use a novel mobile health application (mHEALS) to track patient recovery after major abdominal surgery. Based on feedback from patients and surgeons, we identified areas for improvement in the app, such as streamlining picture uploads. Further study including a randomized, controlled trial is planned and expected to begin enrollment in early 2017.
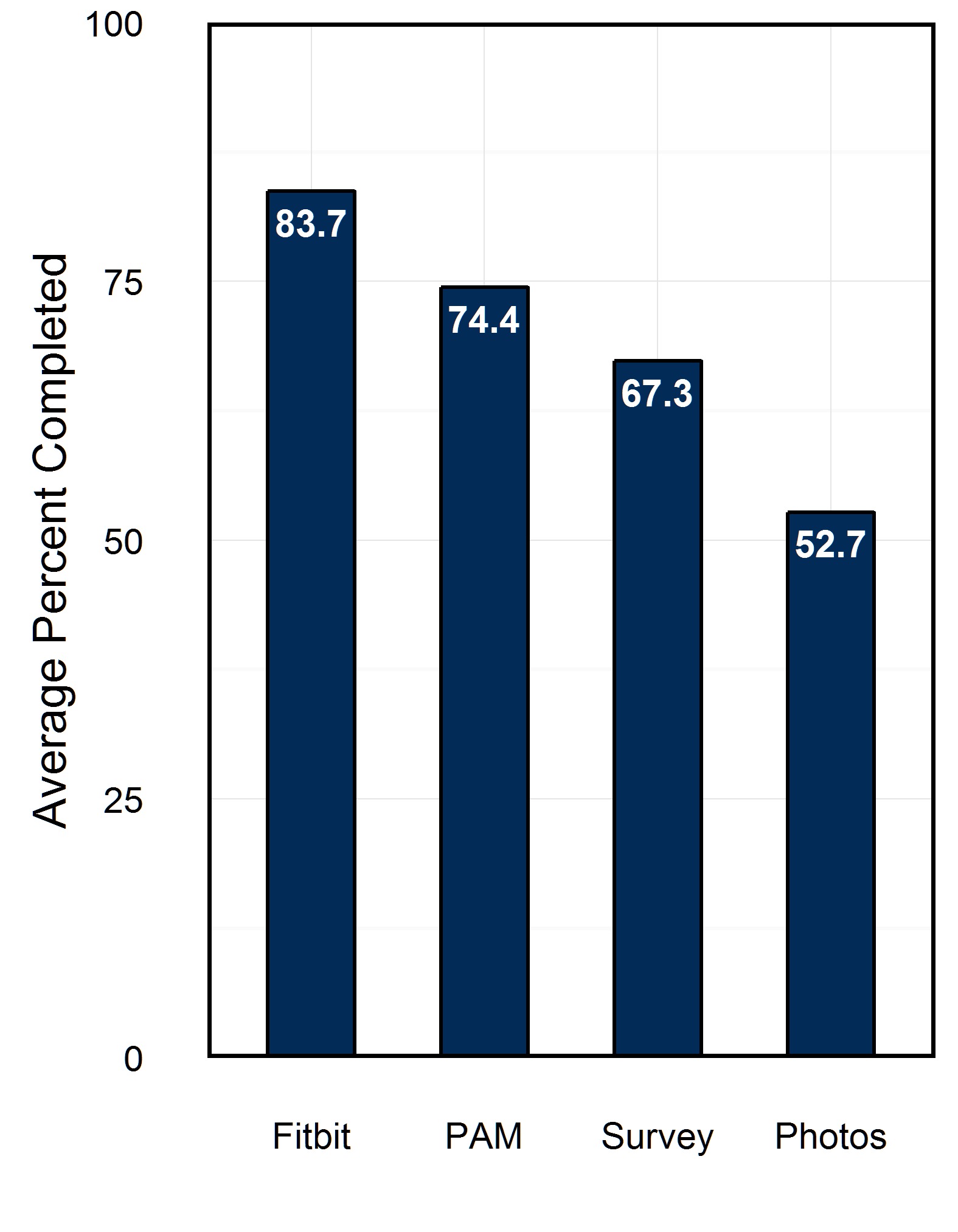
Figure 1. Average task completion within the mHEALS application for FitBit, Photo Affective Meter (PAM), surveys, and photographs
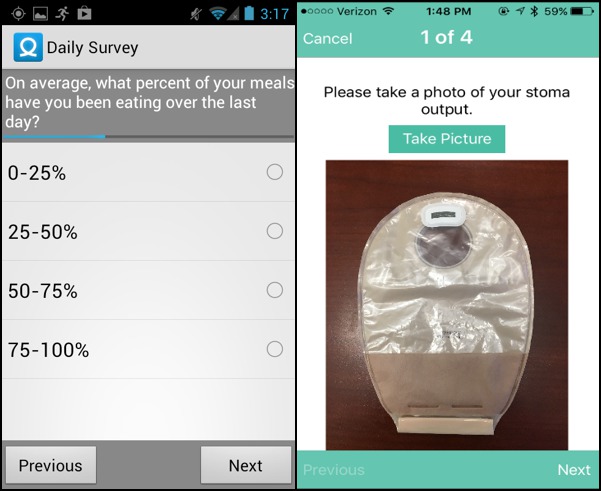
Figure 2. Example screenshots of early iterations of the mHEALS application.
Back to 2017 Program and Abstracts
|