|
Back to 2017 Program and Abstracts
GEOGRAPHIC REGION, SOCIOECONOMIC FACTORS AND CANCER SITE ARE ASSOCIATED WITH VARIATIONS IN PALLIATIVE CARE UTILIZATION FOR ADVANCED GASTROINTESTINAL MALIGNANCIES
Robert H. Hollis*, Lauren Goss, Tyler S. Wahl, Carla N. Holcomb, Melanie Morris, Gregory D. Kennedy, Daniel I. Chu
Surgery, University of Alabama at Birmingham, Birmingham, AL
Introduction: Palliative care is important for promoting quality of life and reducing symptom burden in patients with advanced cancer. The factors influencing variations in palliative care utilization, however, are unclear. We hypothesize that there are significant variations in palliative care utilization by geographic region and socioeconomic status for patients with advanced gastrointestinal (GI) malignancy.
Methods: Patients with clinical stage IV GI malignancies from thirteen cancer sites were identified within the National Cancer Data Base between years 2004-2013. The primary outcome of interest was palliative care utilization defined as care to alleviate symptoms including surgery, chemotherapy, radiation, and/or pain management therapy. Variables of interest included geographic region separated by the US census divisions and median household income for area of residence. Multivariate logistic regression was used to identify predictors of palliative care utilization. Covariates in the model were ranked by relative contribution defined by the chi-square value minus the degrees of freedom.
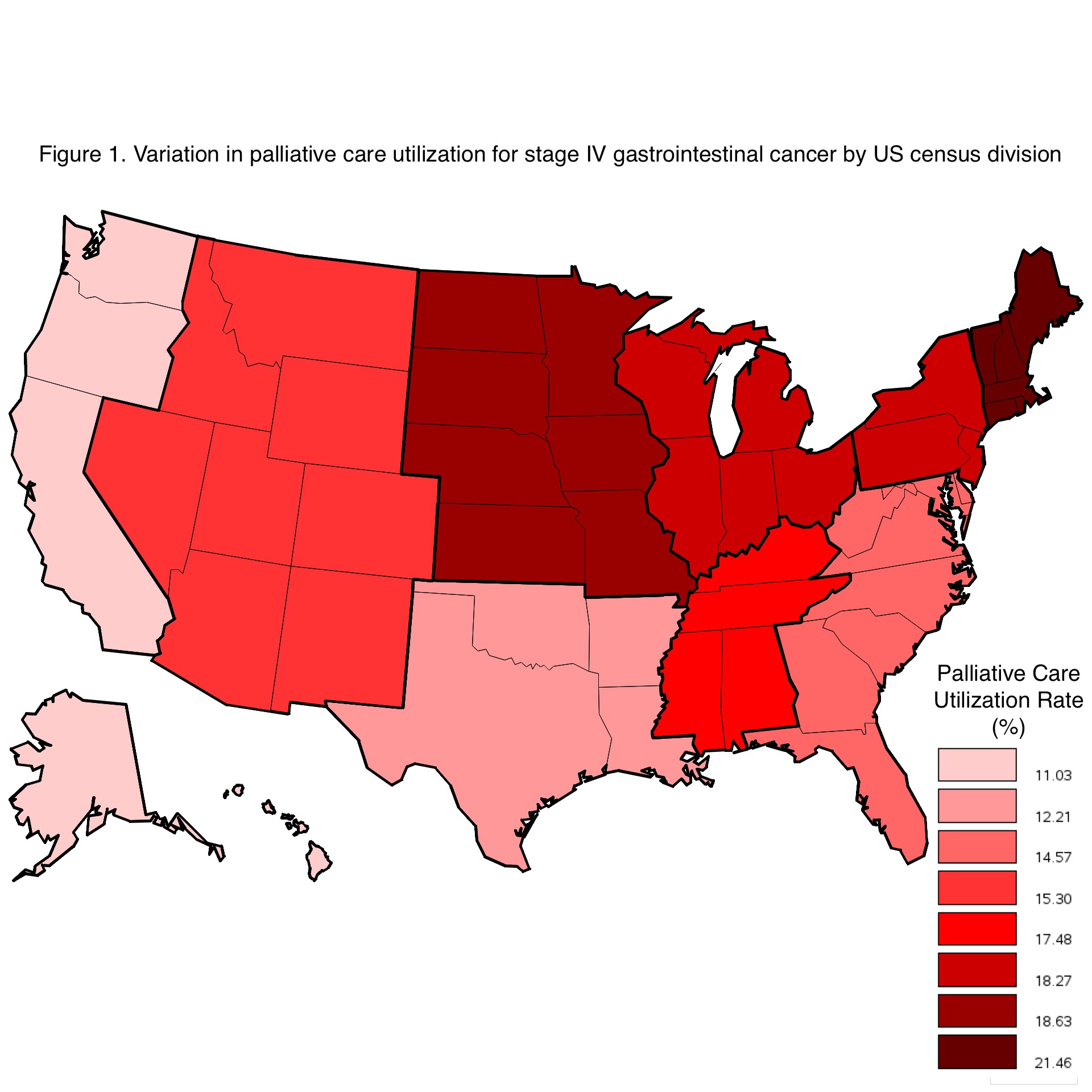
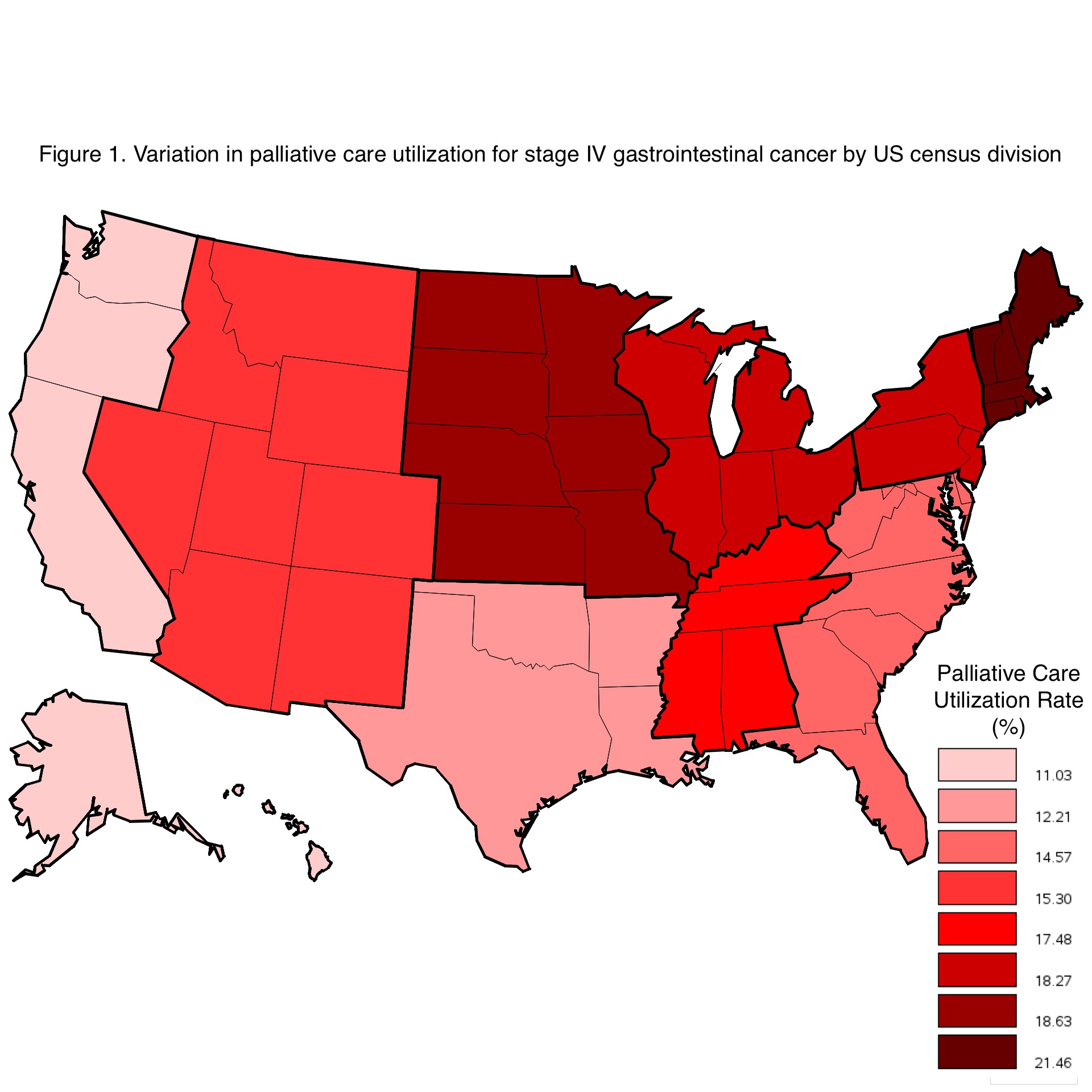
Results: Of 315,597 patients with stage IV GI cancer, 51,201 (16.2%) received palliative care. Palliative care therapy included chemotherapy (34.3%), radiation therapy (16.0%), surgery (15.4%), pain management (12.5%), a combination of therapies (10.0%) and unknown (11.8%). Palliative care use varied by primary cancer site ranging from 25.3% for esophageal cancer to 11.1% for colon cancer. There was significant variation in palliative care use by geographic region with highest utilization in New England (21.5%) and lowest in the Pacific (11.0%) regions (p<0.01; Figure 1). On multivariate analysis, the three most important predictors of palliative care use included primary cancer site, facility location, and income quartile: esophageal cancer was associated with a 2.56 higher odds (95%CI 2.47-2.65) of palliative care use than colon cancer; New England region was associated with a 2.16 higher odds (95% CI 2.04-2.27) of palliative care use than patients in the Pacific region; and areas with a median household income of <$38,000 had a 1.36 higher odds (95% CI 1.31-1.42) of palliative care compared to areas with median income above $63,000.
Conclusion: Geographic region, socioeconomic factors and cancer site are associated with significant variations in palliative care utilization for stage IV GI cancer patients. To promote equitable cancer care, further work is needed to understand the mechanisms driving these variations.
Back to 2017 Program and Abstracts
|