|
 |
Back to 2017 Program and Abstracts
THE EFFICACY OF PERIOPERATIVE FLUID RESTRICTION FOR POSTOPERATIVE COMPLICATIONS AFTER PANCREATODUODENECTOMY
Atsushi Shimizu*, Manabu Kawai, Seiko Hirono, Ken-ichi Okada, Motoki Miyazawa, Yuji Kitahata, Hiroki Yamaue
2nd Department Surgery, Wakayama Medical University, Wakayama, Japan
[Background/Aims] Overload of intraoperative fluid had been often caused to subclinical edema in lungs and the other tissues followed by decreased tissue oxygenation. It results in increasing the postoperative complications including ileus and anastomosis leakage. Recently, Goal-directed fluid therapy (GDFT) has been developed, which may restrict and optimize intraoperative fluid volume. The aim of this study was to evaluate how GDFT affects postoperative complication after pancreaticoduodenectomy (PD).
[Method] GDFT has been introduced since 2013 at a single institution. Two hundred patients underwent PD were enrolled. One hundred patients were classified into liberal fluid management (LFM) group and 100 patients were classified into GDFT group. In this study, the following parameters to evaluate the edema of tissue were used; subtraction of thick of jejunal wall at the pancreatojejunostomy, ventral wall and body trunk, which were measured between preoperative and postoperative (POD4) CT.
[Result]Intraoperative fluid volume was significantly reduced in GDFT group compared to LFM group. There was no difference of the rate of overall complications between both groups (25% v.s. 35%; P=0.123), however, the rate of developing POPF gradeB/C was significantly low in GDFT group (7% v.s.16%, P=0.046). The difference of thick of jejunal wall and body trunk were significantly thinner in GDFT group than that in LFM group (+1.8mm v.s. +2.5mm, P=0.008; +0.6mm v.s. +7.8mm, P=.001). The patients with POPF grade B/C tended to have a more difference of jejunal wall compared to the patients without POPF grade B/C(+3.3mm vs+2.0mm; P=0.06), and the patients with overall complication significantly had a significant difference of ventral wall compared to those without complications (+7.5mm vs+1.9mm; P=0.013).
[Conclusion]The restricted fluid management by GDFT may reduce the complications including POPF by preventing the postoperative tissue edema.
THE RELATIONSHIP BETWEEN MESORECTAL GRADING AND ONCOLOGIC OUTCOMES IN RECTAL ADENOCARCINOMA
Mo1000
THE GI SURGERY JOB MARKET AND ASSESSING NEED FOR A COMPLEX GI SURGICAL FELLOWSHIP
Edward E. Cho*1, Kenric . Murayama2, Matthew M. Hutter3, Frances . Lewis1, D Rohan . Jeyarajah1
1Surgery, Methodist Health System, Dallas, TX; 2Department of Surgery, University at Hawaii, Kaka'ako, HI; 3Department of Surgery, Massachusetts General Hospital, Boston, MA
Introduction
Several surgical organizations have been in collaboration through an Advanced Gastrointestional (GI) Surgery Task Force in an effort to better define advanced GI surgery training and to do a needs assessment of health systems, departments and practice groups interested in hiring a GI surgeon. The aim of this survey is to identify qualifications of prospective job candidates that might be of interest to a GI surgeon.
Method
This is a SSAT sponsored 20-questions survey which was sent out to the Society members in general surgery practices (mix of hospital based and private) across the United States through an online electronic survey software. Descriptive statistics were generated for aggregate survey responses.
Results
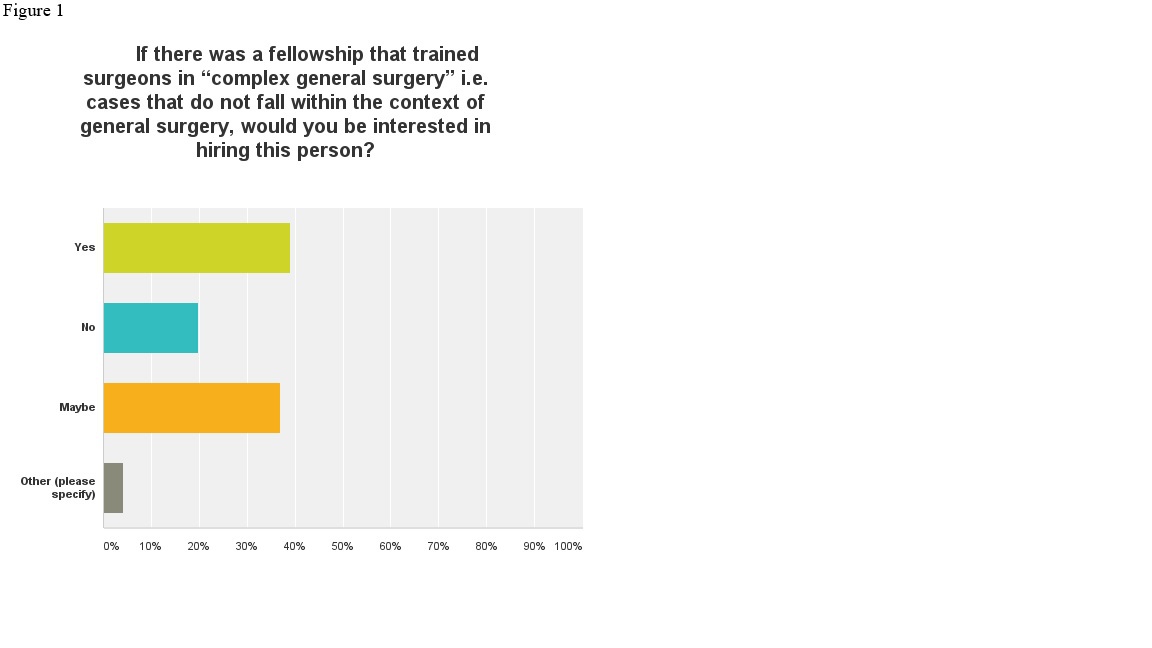
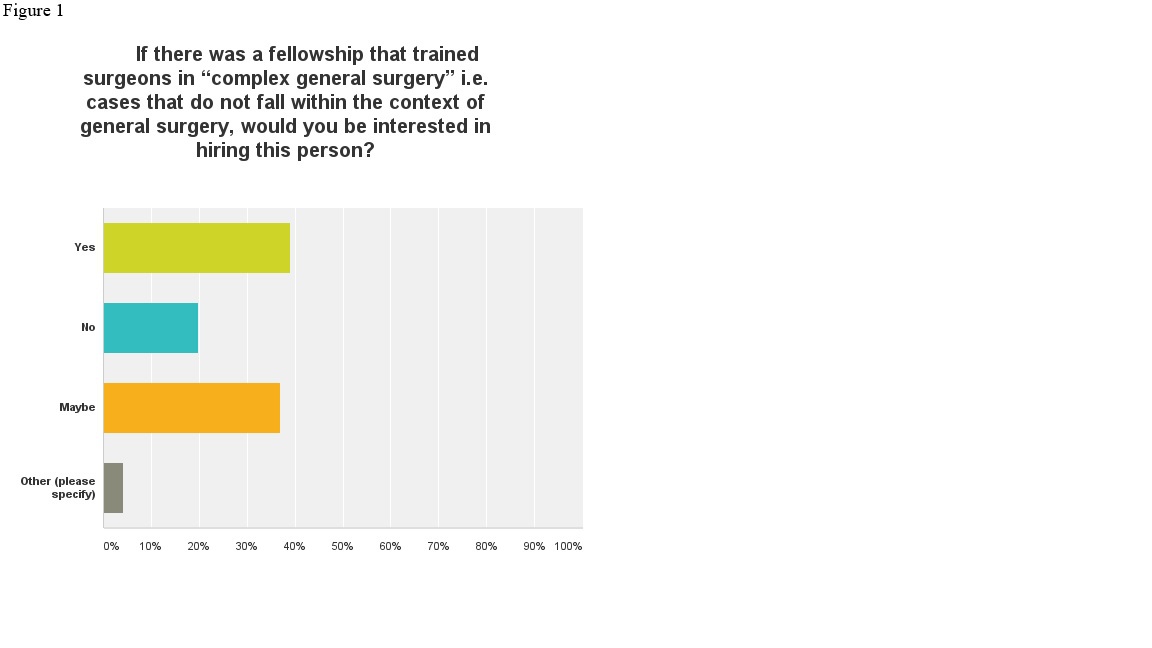
We had a total of 285 responses. Majority (92%) preferred hiring a surgeon who has completed a post graduate fellowship. Type of fellowship preferred by the prospective employers varied depending on the focus and the need of the individual practices. Most important characteristic that the employers sought were personal traits displayed through references, letters of recommendation and work ethic, followed by technical skills, and completion of fellowship. Most of the responders felt that a complex GI surgery fellowship may be an attractive qualification in prospective job candidates (Figure 1).
Conclusion
Our survey showed that the majority of surgery practices in the US prefer fellowship trained candidates as potential hires. Only a small minority (< 20%) of those surveyed felt that completing a “complex general surgery” fellowship would not give prospective candidates an advantage in obtaining a job. Our results indicate a growing need for a complex GI surgery fellowship, especially in light of decreasing exposure and experience of complex cases during surgical residency training.
Mo1001
ERAS IN THE COMMUNITY HOSPITAL: STEPWISE APPROACH TO QUALITY IMPROVEMENT
Shane M. Svoboda*1, Daniel . Galante1, Joann . Coleman1, Karen . Sweeney1, David . Blumberg1, Vanita . Ahuja1,2
1Surgery, Sinai Hospital, Baltimore, MD; 2Sidney Kimmel Medical College, Philadelphia, PA
Introduction: Enhanced recovery after surgery (ERAS) programs have been successful in many academic centers; however, their efficacy in a community hospital remains unclear. A community hospital in Maryland implemented the ERAS protocol for elective colorectal (CR) surgery in January 2015. We hypothesized that a resident-led quality improvement project with a multi-disciplinary team stepwise approach can be established at a community hospital to implement ERAS successfully. Our aim was to reduce hospital length of stay and surgical site infections (SSI).
Method: Baseline data from the American College of Surgeon (ACS)- National Surgical Quality Improvement Program (NSQIP) was used to establish and monitor 30-days postoperative outcomes. A nursing team was educated on ERAS protocol and adherence to each measure. The project was accomplished in 18 months with a bundled approached implemented every six-months. Positive outcomes were initially observed in a limited number of measures. The goal was to continue with the protocol to realize improvement in all measures of the protocol in a stepwise approach to enhance patient outcomes. Continuous monitoring and systematic timely communication of the results were measured and communicated to encourage staff to sustain behavior changes.
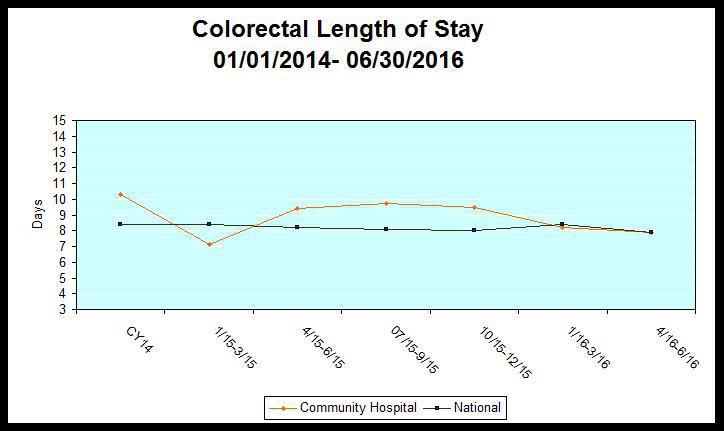
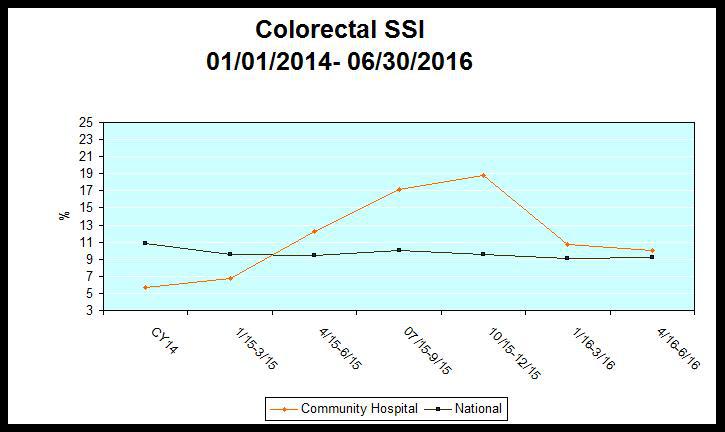
Results: Data was collected on a total of 215 patients over the time period with mean age of 65 years (105 males, 110 females). In the first six months, educational materials were developed and information was disseminated to patients, key stakeholders, and medical staff. ACS-NSQIP data for the base time period (CY2014) when compared to national average was higher for LOS ( 9.5 days vs. 8.7 days) while below for SSI (5.7% vs. 10.8%). The second step was rolled out for the next months with implementation of each measure. The third step was Jan-June 2016 with assessment of compliance of each measure in partnership with nursing. The final data was assessed in August 2016 which showed that our LOS decreased by 15% compared to Jan 2015 (Table 1); while SSI rate increased by 4.6% (Table 2). A quick assessment showed that we had not educated our new surgeons on our wound barrier for SSI prevention. The next step is to educate all staff and reintroduce a CR wound infection bundle to decrease SSI rate.
Conclusion: Concurrent data from ACS-NSQIP can be used to assess performance evaluation and to identify the determinants of outcomes achieved at a community hospital. A stepwise approach can be a successful strategy to implement a complex protocol at a community hospital with reduced resources. This approach helped us to bundle our resources, engage our team to sustain quality improvement while continuing to focus on improving the next quality measure.
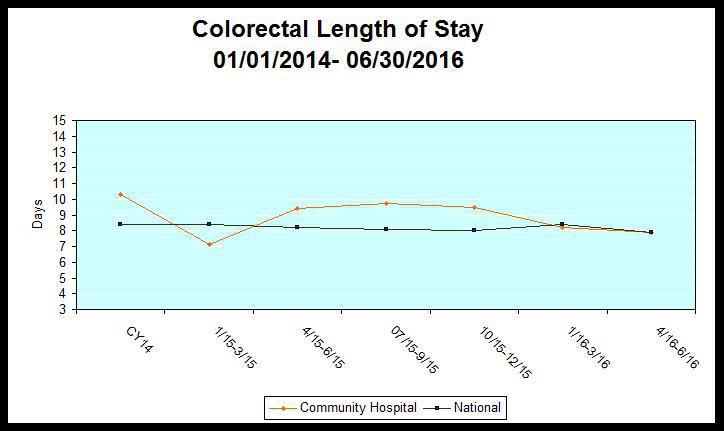
Table 1: Length of Stay in Colorectal Surgery Patients
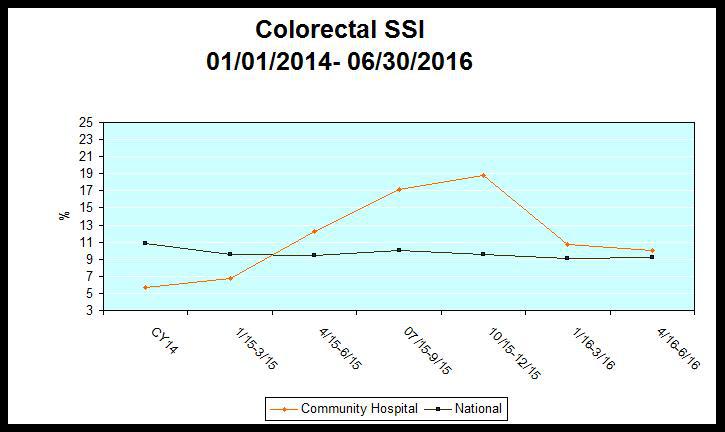
Table 2: Surgical SIte Infection in Colorectal Surgery Patients
Back to 2017 Program and Abstracts
|