|
 |
Back to 2017 Program and Abstracts
NEOADJUVANT CHEMOTHERAPY IS ASSOCIATED WITH HIGHER RATES OF MARGIN NEGATIVE RESECTION AND IMPROVED SURVIVAL IN PATIENTS WITH EXTRAHEPATIC CHOLANGIOCARCINOMA
Andrew J. Benjamin*1, Nicholas R. Suss2, Kevin K. Roggin1, David J. Bentrem3, Mark S. Talamonti2, Marshall S. Baker2
1Surgery, University of Chicago Medical Center, Chicago, IL; 2Surgery, Northshore University Healthsystem, Evanston, IL; 3Surgery, Northwestern University, Chicago, IL
Background
Few studies have investigated the clinical value of neoadjuvant chemotherapy in the management of patients with resectable extrahepatic cholangiocarcinoma (EH-CCA).
Methods
We queried the National Cancer Database to identify patients undergoing resection for clinical stage I-III EH-CCA between 2004 and 2013. Patients with metastatic disease and those undergoing R2 resections were excluded. Multinomial logistic and multivariable Cox regression models controlling for demographics, comorbidity burden, pre-treatment clinical stage, and chemotherapy regimen were used to identify predictors of a margin positive (R1) resection, and to identify clinical differences, and compare overall survival between three cohorts: patients undergoing resection with no chemotherapy, those undergoing neoadjuvant chemotherapy prior to resection and those undergoing resection followed by adjuvant chemotherapy.
Results
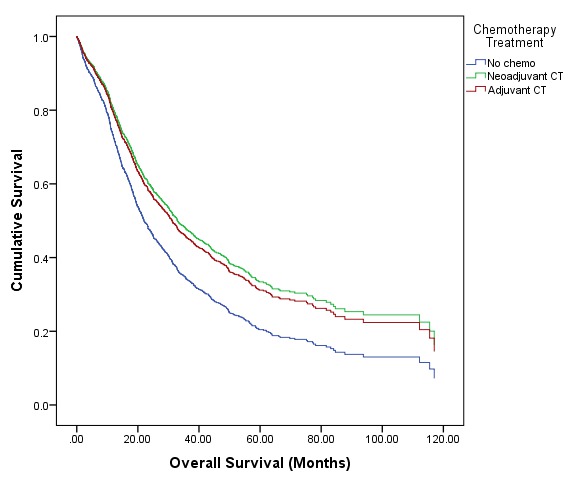
1,653 patients met inclusion criteria. 830 (50.2%) received no chemotherapy, 84 (5.1%) received neoadjuvant chemotherapy, and 739 (44.8%) received adjuvant chemotherapy. On multinomial regression there were no differences in age, demographics, comorbidity burden, and pretreatment clinical stage between patients receiving neoadjuvant chemotherapy and those receiving adjuvant chemotherapy. Compared to patients receiving no chemotherapy, patients receiving any chemotherapy were less likely (p<0.001) to be of advanced age (≥75 years old) and more likely to have advanced clinical stage (p<0.04). On multivariable regression, African American race (OR 1.860 [1.028, 3.367], p=0.04), tumor size ≥3 cm (OR 5.195 [1.792, 15.057], p=0.002), and receiving no chemotherapy prior to surgery (OR 1.698 [1.228, 2.348], p=0.001) were predictors of R1 resection. Overall survival varied by treatment (Figure 1). Patients who did not receive chemotherapy had a median survival of 18.8 months compared to 38.7 months for patients undergoing neoadjuvant chemotherapy prior to resection (HR 0.641 [0.476, 0.864], p=0.004), and 28.9 months for patients undergoing adjuvant chemotherapy following resection (HR 0.726 [0.640, 0.824], p<0.001). Multivariable Cox regression identified stage III disease (HR 1.65 [1.344, 2.026], p<0.001), and R1 resection (HR 1.738 [1.482, 2.039], p<0.001) as independent determinants of survival conferring risk of death. Adjuvant (HR 0.734 [0.636, 0.848], p<0.001) and neoadjuvant chemotherapy (HR 0.691 [0.499, 0.956], p=0.026) were identified as independent predictors of improved survival.
Conclusions
Neoadjuvant chemotherapy appears to be associated with improved rates of margin negative resection and overall survival in patients with EH-CCA. The value of neoadjuvant treatment in patients with resectable EH-CCA should be the subject of future randomized trials.
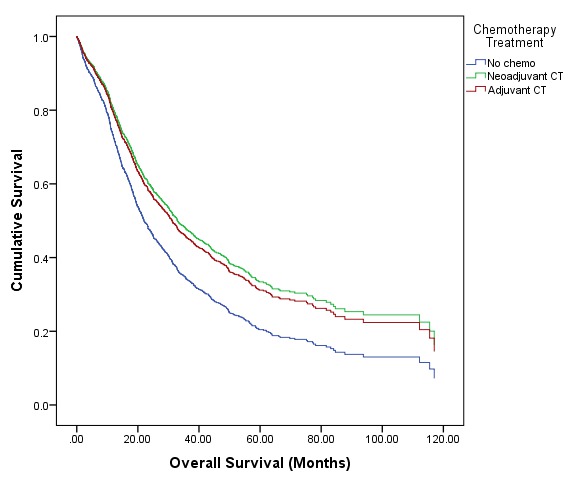
Figure 1: Cox proportional hazard model of overall survival stratified by chemotherapy regimen in patients undergoing resection for EH-CCA. The Cox model was adjusted for patient age, demographics, comorbidity burden, clinical stage, and chemotherapy regimen.
Back to 2017 Program and Abstracts
|