|
 |
Back to 2017 Program and Abstracts
THE IMPACT OF ADJUVANT THERAPY DELAY ON SURVIVAL FOLLOWING PANCREATICODUODENECTOMY FOR PANCREATIC ADENOCARCINOMA
Onur Kutlu*1, Jeffrey E. Lee2, Nestor de La Cruz1, Claudius Conrad2
1Surgery, University of Miami, Miller School of Medicine, Doral, FL; 2Surgical Oncology, University of Texas, MD Anderson Cancer Center, Houston, TX
Background: Adjuvant chemotherapy (AC) or chemoradiation (ACRT) following resection of pancreatic adenocarcinoma (PAC) has been shown to improve survival. However, controversy exists (1) regarding the role of adjuvant therapy when a delay in delivery cannot be avoided due to postoperative complication or prolonged recovery, and (2) whether AC or ACRT represents the superior adjuvant strategy following a margin-positive vs. -negative resection. We leveraged a large administrative database to investigate temporal and comparative effects of AC and ACRT following pancreaticoduodenectomy (PD) for PAC.
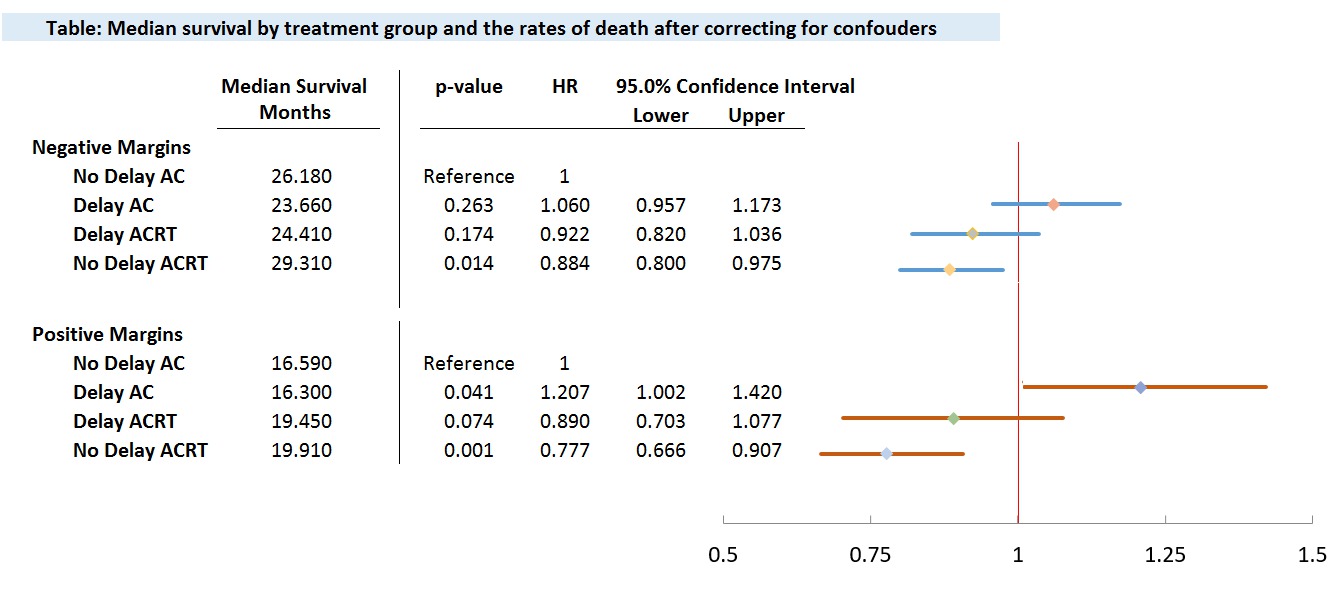
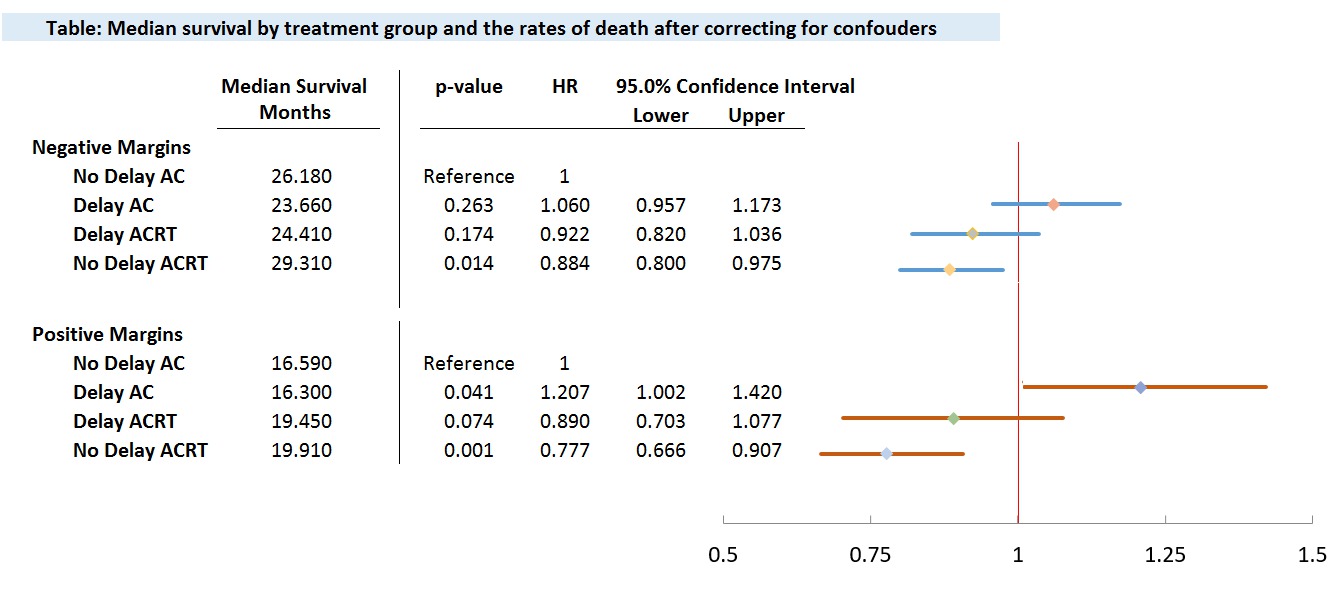
Material and Methods: National Cancer Database (NCDB) identified patients with PAC who underwent PD between 2010-2014. Patients with incomplete clinical data, those who received neoadjuvant therapy or did not receive adjuvant therapy were excluded. The four comparison groups were: (1) <60 days to AC (No Delay AC), (2) <60 days to ACRT (No Delay ACRT), (3) ≥60 days to AC (Delay AC), (4) ≥60 days to ACRT (Delay ACRT). Kaplan-Meier survival analyses were performed for the entire cohort as well as for margin-positive and -negative subgroups. Cox multivariable regression analyses adjusted for confounding factors.
Results: Among 6662 patients, the median follow-up was 20.5 months. Median overall survival (OS) was 23.7 months. Delay of ≥60 days to AC occurred in 39.1%. For margin-negative patients, median OS for Delay AC, Delay ACRT, No Delay AC, No Delay ACRT were 23.6, 24.4, 26.1, 29.3 months respectively. For margin-positive patients, median OS for Delay AC, Delay ACRT, No Delay AC, No Delay ACRT were 16.3, 19.5, 16.6, 19.9 months respectively. For the entire cohort, a trend toward improved survival was seen between No Delay vs. Delay AC, 30.8 vs. 28.9 months, p=0.056, HR 1.067, 95% CI 0.998-1.141). While No Delay vs. Delay AC afforded no survival benefit to the margin-negative cohort (p=0.263), No Delay AC vs. Delay AC showed survival benefit among margin-positive patients after correcting for confounders (16.6 vs 16.3 months; p=0.041, HR 0.845, 95% CI 0.704-0.998). In contrast, among margin-positive patients, No Delay vs. Delay ACRT was associated with statistically identical outcome (19.9 vs 19.4 months, p=0.054).
Conclusion: Margin-negative vs. -positive PAC patients appear to receive differential benefit from AC vs. ACRT after PD, and may be differentially sensitive to delay of adjuvant therapy. In particular, delay of AC ≥60 days may be associated with worse survival in margin-positive patients. This negative effect was not observed among margin-positive patients with a delay of ACRT ≥60 days. Consideration should be given to deliver ACRT rather than AC in margin-positive patients when delay of adjuvant therapy ≥60 days cannot be avoided.
Back to 2017 Program and Abstracts
|