|
 |
Back to 2017 Program and Abstracts
PERCEIVED VS. ACTUAL BENEFIT: A NATIONAL ANALYSIS OF THE SURGERY-FIRST APPROACH FOR RESECTABLE PANCREATIC CANCER
John R. Bergquist*1,3, Christopher R. Shubert1,3, Tommy Ivanics3, Santhi Swaroop Vege2, David M. Nagorney1, Michael L. Kendrick1, Michael B. Farnell1, Rory Smoot1, Elizabeth B. Habermann3, Mark J. Truty1
1Surgery, Mayo Clinic, Rochester, MN; 2Gastroenterology, Mayo Clinic, Rochester, MN; 3Kern Center for the Science of Healthcare Delivery, Mayo Clinic, Rochester, MN
Background: Surgical resection is necessary for long-term survival in pancreatic adenocarcinoma (PDAC) and is perceived as the optimal initial treatment strategy in patients with “resectable” tumors. However, three critical factors are necessary for maximal survival benefit: (A) negative margin resection, (B) absence of metastatic disease, and (C) adjuvant chemotherapy. We sought to determine the combinatorial frequency of these critical factors and their effect on survival outcomes after a surgery-first approach in localized PDAC using national retrospective outcomes data.
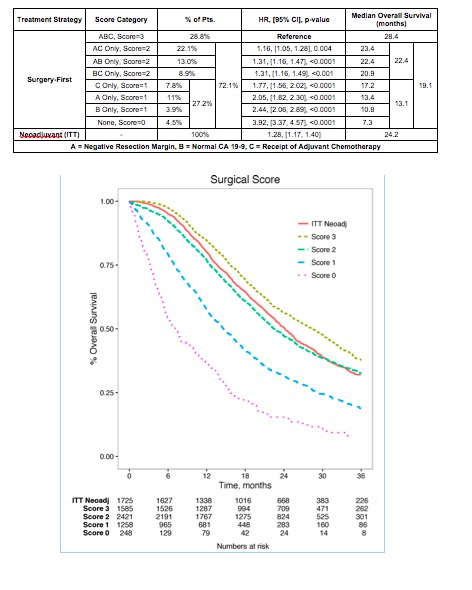
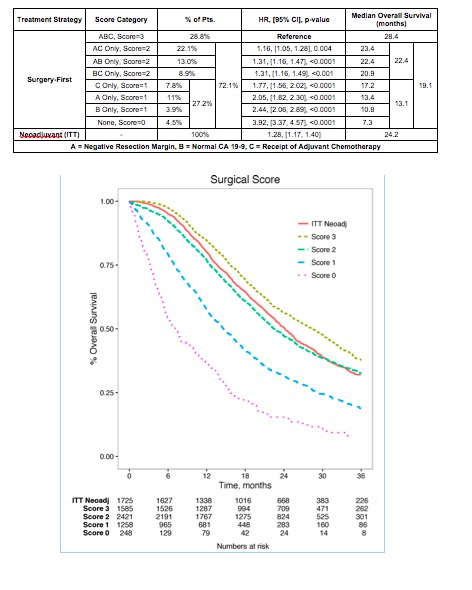
Methods: The National Cancer Data Base (NCDB) 2009-2012 was reviewed for patients with early stage (I/II) anatomically resectable PDAC undergoing curative intent resection and assessed for: (A) negative margins, (B) normal pre-op CA19-9 levels (surrogate for absence of occult metastases), and (C) receipt of adjuvant chemotherapy. Patients receiving surgery-first were scored based on presence (score=1) or absence (score = 0) of combinations of these factors (total score=0-3) and overall survival (OS) was analyzed by various factor combinations. We then compared these outcomes with patients receiving neoadjuvant therapy on an intention to treat (ITT) basis, including those that did not subsequently undergo surgery.
Results: 7,249 total patients were assessed (n = 5,512 surgery-first, n = 1,737 ITT neoadjuvant). Unadjusted survival decreased with each failing factor and varied by specific factor combinations, this persisted even after adjustment (Figure). Only 28.8% of patients undergoing surgery-first approach were able to achieve an ideal score (3) that was associated with greatest survival benefit (OS=29.1 months). A similar proportion (27.2%) achieved the lowest scores (0 or 1) and resulted in the lowest survival (OS=13.1 months). For comparison, the entire ITT neoadjuvant therapy cohort, including those who did not ultimately undergo resection, realized overall survival outcomes (24.2 months, log rank p<0.001), that were superior to 71.2% of the surgery-first patients (score ≤ 2).
Conclusion: Survival decreases with each failing factor and is cumulatively contingent by specific factor combinations that cannot be guaranteed prior to resection. Despite the perception of optimal benefit from a surgery-first approach in seemingly “resectable” PDAC, only 1 in 3 patients are ultimately able to achieve maximal survival benefit. Patients are equally likely to have the worst suvival outcomes with a surgery-first strategy. Similarly staged patients undergoing neoadjuvant therapy (including those not resected) can achieve survival outcomes that are superior to the majority of those undergoing a surgery-first approach. Further investigation is needed to critically re-assess our perception of benefit versus actual outcomes with a surgery-first sequence strategy in resectable PDAC.
Back to 2017 Program and Abstracts
|