|
 |
Back to 2017 Program and Abstracts
TUMOUR SIZE IS NOT A RELIABLE CRITERION FOR RESECTION OF PATIENTS WITH NON-SECRETING PANCREATIC NEUROENDOCRINE TUMOURS: RESULTS OF AN INTERNATIONAL, MULTI-CENTRE, OPERATIVE COHORT
Logan Mills1, Panagiotis Drymousis2, Yogesh Vashist3, Christoph Burdelski3, Andreas Prachalias1, Parthi Srinivasan1, Krishna Menon1, Saboor Khan4, Judith Cave5, Thomas Armstrong5, Martin O. Weickert4, Andrea Frilling2, John K. Ramage1, Raj Srirajaskanthan*1
1ENETS Centre of Excellence, King's College Hospital NHS Foundation Trust, London, United Kingdom; 2ENETS Centre of Excellence, Imperial College Healthcare NHS Trust, London, United Kingdom; 3Department of General, Visceral and Thoracic Surgery, University Medical Centre Hamburg-Eppendorf, Hamburg, Germany; 4ENETS Centre of Excellence, University Hospitals Coventry and Warwickshire NHS Trust, Coventry, United Kingdom; 5ENETS Centre of Excellence, University Hospital Southampton NHS Foundation Trust, Southampton, United Kingdom
Background
Small pancreatic neuroendocrine tumours (pNETs) present a management dilemma because of their uncertain natural history. Surveillance studies of tumours ≤2cm show minimal tumour growth, but up to 4% incidence of metastases and only 3 years of follow-up on average (Partelli, 2016). By contrast, the most recent WHO classification system regards all pNETs as potentially malignant. Surgical resection is the only potentially curative treatment.
Aim
To assess the malignant characteristics of small pNETs in a large, retrospective, multicentre, operative patient cohort.
Methods
Patients were identified from five European hospitals using inclusion criteria of non-functional, non-familial, resected pNETs of all stages and grades. Logistic regression for clinical, biochemical and pathological variables, and cox regression for survival data, were performed using SPSSv22.
Results
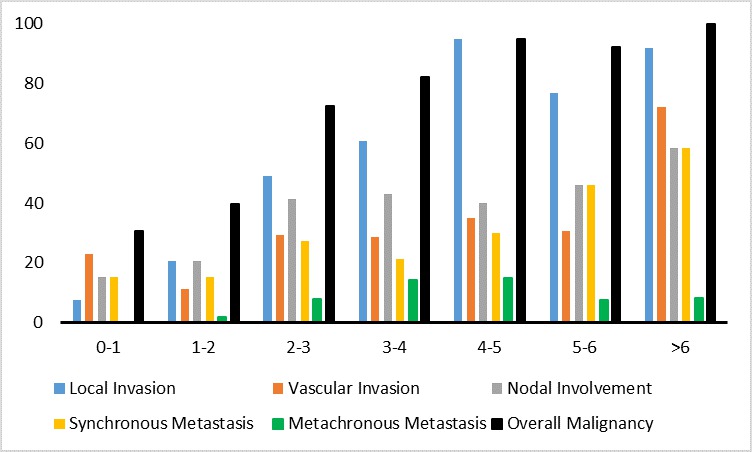
227 patients with a resected pNET were identified. 66 (29%) had tumours ≤2cm. Surgical procedures included 83 Whipple’s resections, 133 distal pancreatectomies, 8 enucleations and 3 total pancreatectomies. Malignancy was defined as any of local, vascular or lymphatic invasion or distant metastasis. Overall, malignancy was confirmed in 165 (73%) patients; 25 (38%) tumours ≤2cm were malignant, compared to 140 (87%) >2cm, p<0.001 (Figure 1). Tumours ≤2cm were staged as stage I:39, II:6, III:11 IV:10. The smallest primary with nodal metastasis was 6mm and with liver metastasis, 10mm. ROC analysis showed that malignancy was identified with 84% sensitivity using the current cut-off of 20mm (AUC 0.823), 91% using 15mm and 97% using 10mm. Prediction of malignancy was not possible in tumours ≤2cm as logistic regression revealed no association between malignancy and diameter, symptomatic presentation, Ki67 or CgA.
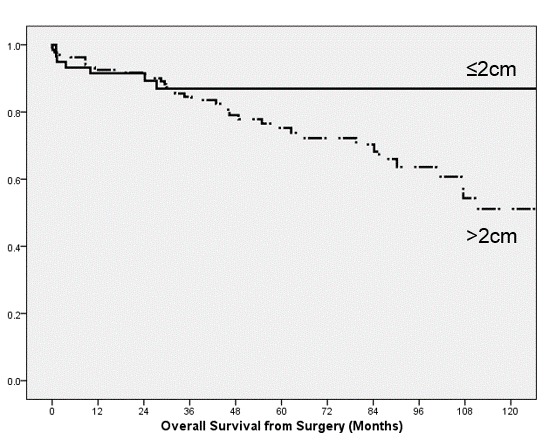
The median survival of this entire cohort was 202 months, and did not significantly differ across the 2cm threshold (p=0.122; Figure 2). Significant prognostic factors for the whole cohort included stage, grade and extrahepatic disease; grade and extrahepatic disease remained significant in multivariate analysis after correcting for age and year of surgery. Importantly, diameter was predictive of progression in all tumour diameters (p<0.001) but not for tumours ≤2cm (p=0.111), and not predictive of overall survival for all diameters (p=0.268), suggesting a shared tumour biology.
Conclusions
1. 38% of pNETs ≤2cm displayed malignant features.
2. Metastatic disease was reported in primaries as small as 6mm; the current surveillance cut-off of 20mm would miss 9% of malignancy.
3. Survival was not significantly better for tumours ≤2cm than for tumours >2cm, reflecting the malignant potential shared by all pNETs.
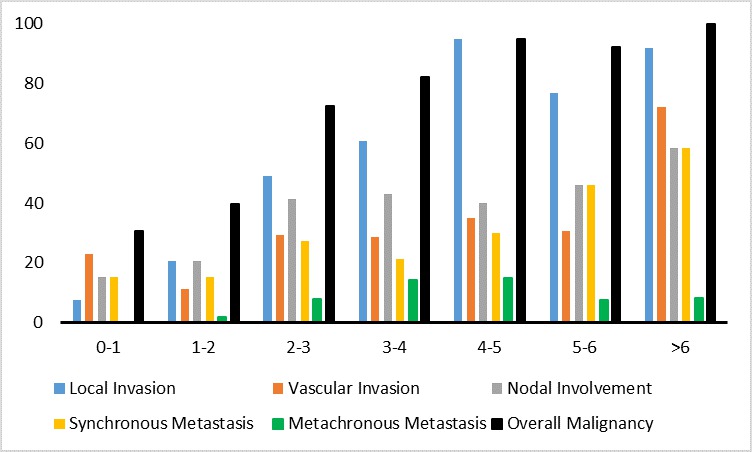
Figure 1 Prevalence of malignant features (%), stratified by tumour diameter (cm).
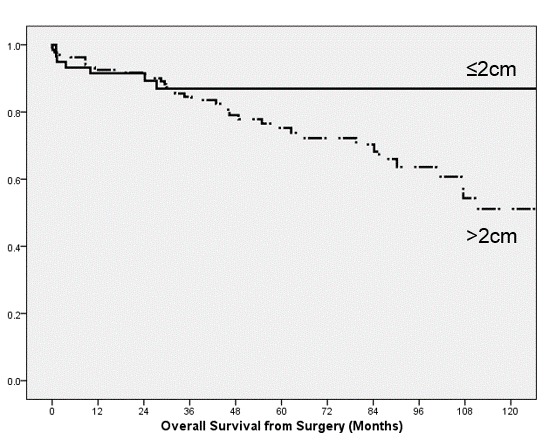
Figure 2 Kaplan-Meier survival curves of 193 patients with >12 months follow-up, stratified by tumour diameter. p=0.122
Back to 2017 Program and Abstracts
|