|
Back to 2017 Program and Abstracts
ADEQUATE LYMPHADENECTOMY IN SMALL BOWEL NEUROENDOCRINE TUMORS: ANALYSIS OF THE NCDB
Benjamin M. Motz*, Patrick D. Lorimer, Kendall Walsh, I'sis N. Perry, Joshua S. Hill, Jonathan C. Salo
Surgery, Carolinas Medical Center, Charlotte, NC
Introduction
Neuroendocrine tumors (NETs) are most commonly found in the small bowel and have been shown to have high rates of nodal and distant metastasis. Current NCCN guidelines for resection of small bowel NETs recommend regional lymphadenectomy (LAD). However, no consensus exists on the extent of LAD required for accurate staging or improved survival.
Methods
The NCDB was queried for patients with small bowel NETs undergoing resection (1998-2013). Patients with distant metastases and incomplete pathologic staging were excluded. Cut-point analysis was performed to stratify groups of patients by likelihood of nodal positivity. This was done by determining the maximal Chi-square statistic between consecutive numbers of nodes resected, and then dividing our cohort in two groups. Multivariable survival analysis was performed using a Cox proportional hazards model with stepwise selection.
Results
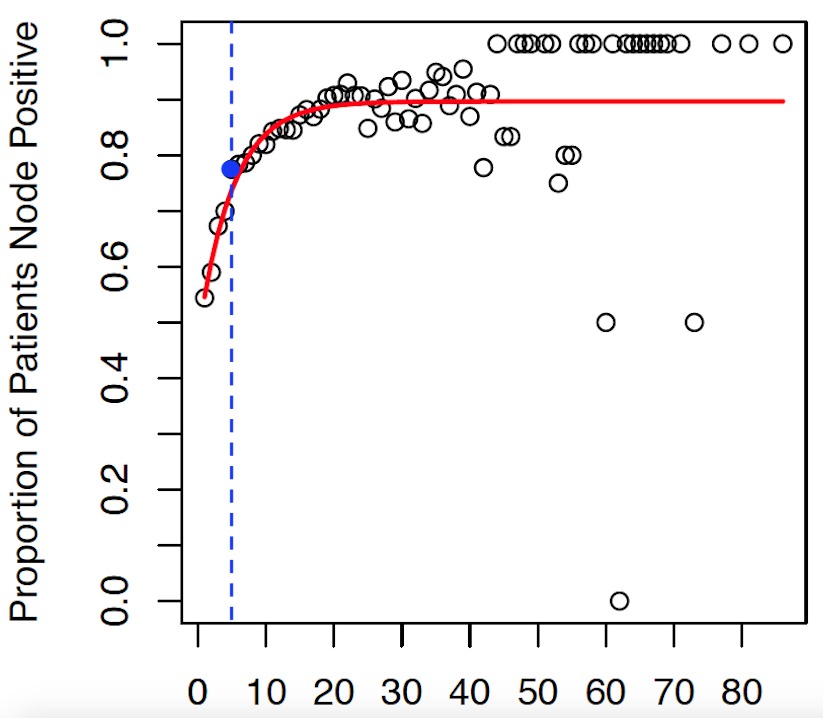
12203 patients were identified: 7050 (57.8%) ileal; 4046 (33.2%) small bowel, not otherwise specified (NOS); 737 (6.0%) jejunal; 227 (1.9%) overlapping areas of small bowel; and 143 (1.2%) Meckel’s. Median tumor size was 1.7cm. 7944 (65.1%) patients were node positive (N+). Median LAD was 8 nodes. Cut-point analysis identified the greatest difference in likelihood of nodal positivity when ≥5 nodes were resected (Figure 1). For LAD of ≥5 nodes, more than 77% were N+. Univariate analysis of patients with LAD of ≥5 nodes showed significant survival advantage over those with <5 nodes (p<0.001). On multivariable analysis, significant predictors of survival included: age, gender, race, insurance status, comorbidities and removal of ≥5 nodes (Table 1). Subgroup analysis showed that in patients with <5 nodes resected, nodal positivity and number of positive nodes were significant predictors of survival while tumor size was not significant. For patients with ≥5 nodes resected, tumor size was a significant predictor of survival, while nodal positivity was not significant. Metastatic lymph node ratio, the number of positive nodes divided by number of resected nodes, was a significant predictor of survival after removal of both <5 nodes (HR=1.46, 95%CI=1.09-1.96) and ≥5 nodes (HR=1.39, 95%CI=1.02-1.90).
Conclusions
Patients in the NCDB undergoing resection of small bowel NETs have high rates of nodal metastasis. Our findings indicate that LAD of 5 nodes results in the greatest actuarial increase in likelihood of identifying positive nodes, and should therefore be considered the minimum necessary for accurate staging. Failure to resect at least 5 nodes risks leaving positive nodes in situ. Furthermore, LAD of at least 5 nodes is associated with improved survival. Finally, metastatic lymph node ratio may be useful in predicting survival in patients with small bowel NETs.
Table 1: Multivariable Survival Analysis
| | Cox Proportional Hazards | | Covariate | Hazard Ratio | 95% Confidence Interval | | Age at Diagnosis* | 1.07 | 1.06 - 1.08 | | Gender | | | Male | referent | | Female* | 0.78 | 0.69 - 0.88 | | Race | | | White | referent | | Black* | 1.32 | 1.12 - 1.57 | | Other | 0.84 | 0.52 - 1.34 | | Tumor Location | | | Jejunum | referent | | Ileum | 0.98 | 0.76 - 1.26 | | Meckel | 1.05 | 0.58 - 1.90 | | Overlapping Area of Small Bowel | 1.37 | 0.87 - 2.14 | | Small Bowel, NOS | 1.21 | 0.95 - 1.54 | | Insurance Status | | | Private | referent | | Medicaid* | 2.69 | 1.99 - 3.65 | | Medicare* | 1.42 | 1.20 - 1.69 | | Uninsured* | 1.78 | 1.14 - 2.78 | | Other Government | 1.42 | 0.70 - 2.87 | | Charlson-Deyo Score* | 1.50 | 1.38 - 1.63 | | Tumor Size | 1.00 | 1.00 - 1.00 | | Nodes Resected | | | <5 Nodes | referent | | ≥5 Nodes* | 0.91 | 0.84 - 0.99 |
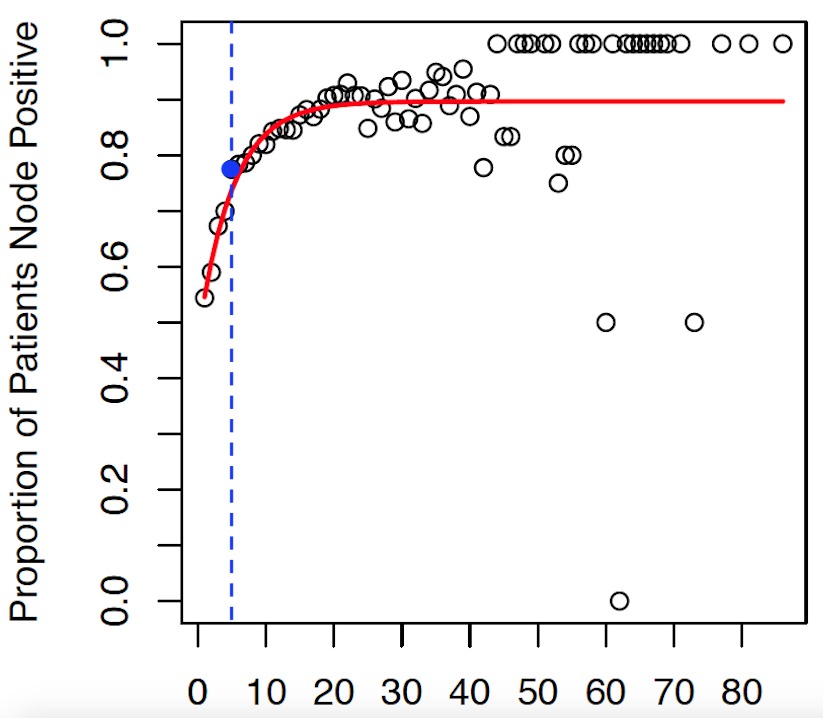 Figure 1: Cut-point analysis using maximal Chi-square identified the greatest actuarial increase in likelihood of nodal positivity between <5 nodes and ≥5 nodes.
Back to 2017 Program and Abstracts
|