|
Back to 2017 Program and Abstracts
INCREASED METABOLIC BENEFIT FOR ELDERLY PATIENTS UNDERGOING ROUX-EN-Y GASTRIC BYPASS VS SLEEVE GASTRECTOMY FOR MORBID OBESITY
Katherine D. Gray*, Maureen D. Moore, Gregory Dakin, Rasa Zarnegar, Alfons Pomp, Cheguevera Afaneh
Surgery, New York Presbyterian Hospital - Weill Cornell Medicine, New York, NY
Background
Elderly patients with morbid obesity and metabolic syndrome are at high-risk for end-organ complications. It is not well studied whether bariatric surgery can improve the metabolic profile of these patients. We sought to assess outcomes at intermediate follow-up in a cohort of elderly patients undergoing laparoscopic sleeve gastrectomy (LSG) or laparoscopic Roux-en-Y gastric bypass (LRYGB).
Methods
A retrospective review was conducted of all patients ≥ age 60 undergoing LSG or LRYGB at our institution between 2007-2014. Patients with prior bariatric operations were excluded. Demographics, body mass index (BMI), American Society of Anesthesiology (ASA) score, metabolic comorbidities, and operative details were collected. Post-operative complications were scored as major if ≥ Clavien-Dindo class 3. Comorbidity resolution was measured by number of oral medications for diabetes mellitus (DM), hypertension (HTN), and hyperlipidemia (HL). Percent total weight loss (%TWL) was also measured.
Results
A total of 134 patients who underwent LSG (n=65) or LRYGB (n=69) were identified. There were no statistical differences between groups with respect to age (mean 64, range 60-75), BMI (mean 44.0 +/- 6.1), or ASA score (88.7% ≥ ASA 3). There was a high rate of metabolic comorbidities; 90.3% had HTN and 76.1% had HL (p not significant between groups). More patients undergoing LRYGB were diabetic (68.1% LRYGB vs 50.8% LSG, p = 0.04).
Between LSG and LRYGB, there were no statistical differences in intraoperative complications (0 LSG vs 2, 2.9% LRYGB; p = 0.17) or major postoperative complications (3, 4.7% LSG vs 4, 5.8% LRYGB; p = 0.75). Mean length of stay was slightly shorter for LSG, 3.1 +/- 1.6 days vs 3.7 +/- 1.4 days for LRYGB, p = 0.02). Readmission rates were not statistically different (3, 4.6% LSG vs 6, 8.7% LRYGB; p = 0.35). There was one stricture (1.4%) in the LRYGB group, and no leaks or mortalities in either group.
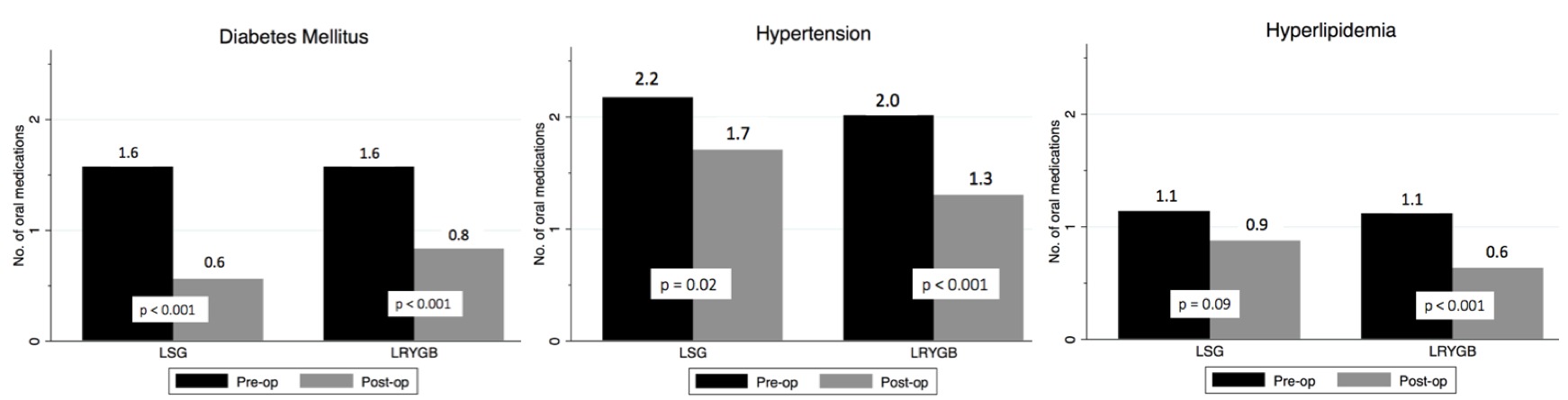
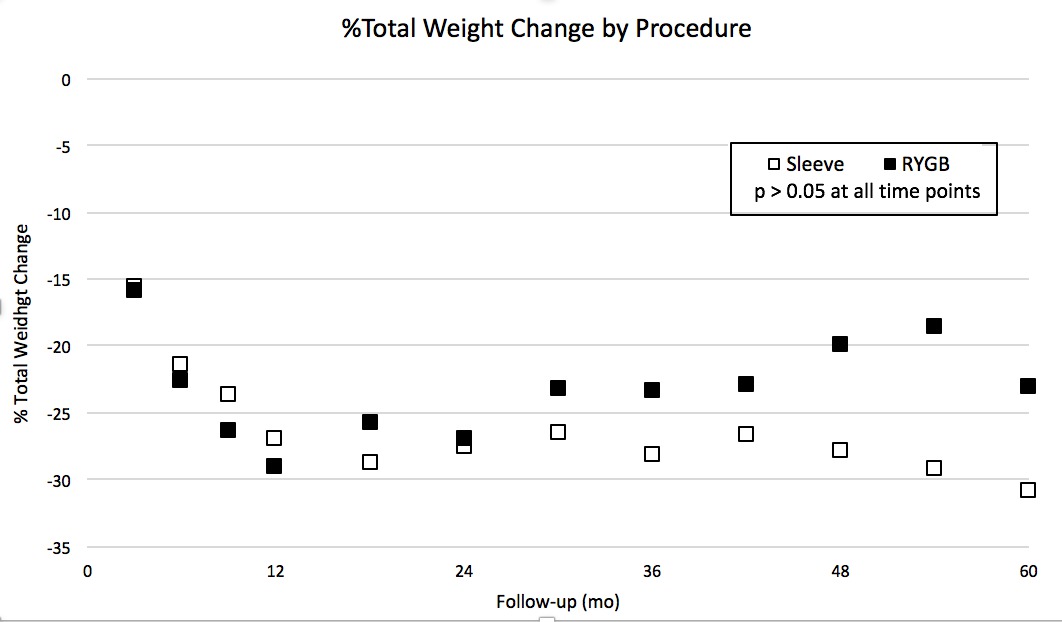
Median follow-up was 25.5 months (IQR 10.5 - 50 months). Patients undergoing LRYGB had improvement in each of DM, HTN, and HL (Figure 1), as well as a significant decrease in mean hemoglobin A1c (7.8 pre-operatively to 6.7 post-operatively, p < 0.001) and insulin use (16/47, 34.0% pre-operatively vs 7/47, 15.2% post-operatively, p = 0.001). Patients undergoing LSG had improvement in DM and HTN but not HL; there was no reduction in insulin dependence for diabetic patients after LSG. Weight loss was not significantly different between groups (Figure 2), with average %TWL at 24 months 27.5% after LSG and 26.9% after LRYGB (p = 0.83).
Conclusion
Both LSG and RYGB can be performed on morbidly obese, elderly adults with acceptable complication rates despite substantial comorbidities. At intermediate follow-up, there is increased metabolic benefit for elderly patients undergoing LRYGB over LSG, especially in patients with insulin-dependent DM.
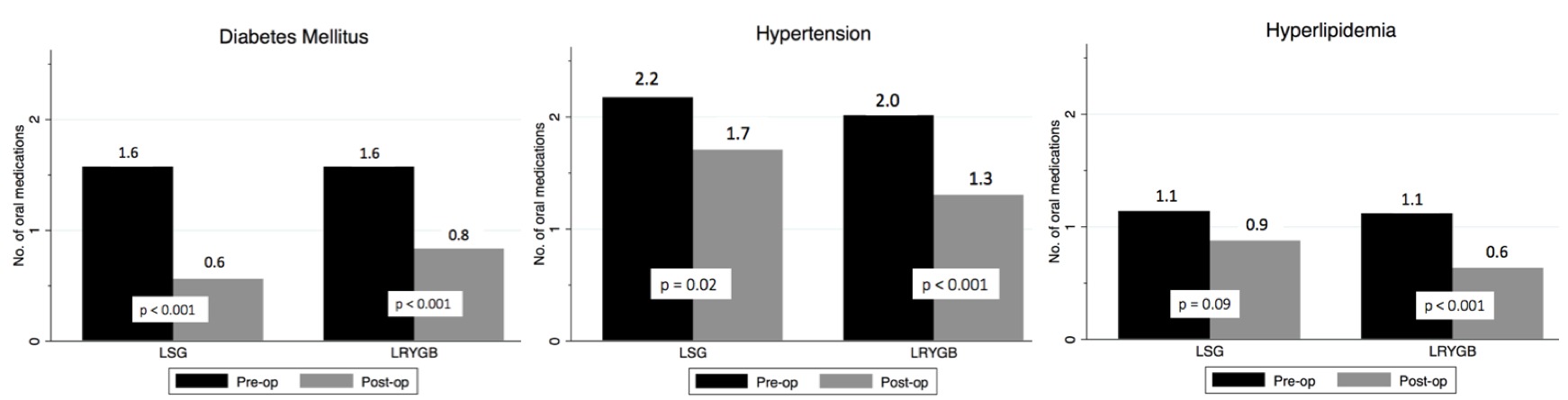
Figure 1. Comorbidity resolution by procedure
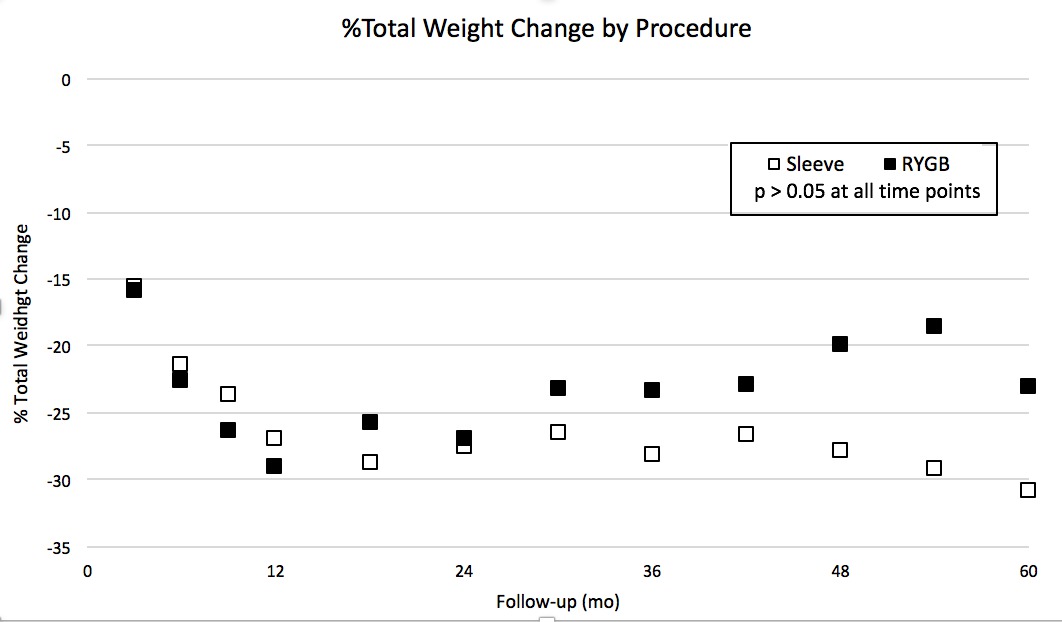
Figure 2. %Total weight change by procedure
Back to 2017 Program and Abstracts
|