|
Back to 2015 Annual Meeting Program
Identification of Prognostic Factors Following Resection of Colorectal Liver Metastases in the Modern Era of Treatment
Cynthia Miller*, Kshitij Arora, Shadi Razmdjou, Vikram Deshpande, Jing Zhao, David L. Berger, Kenneth Tanabe, Keith D. Lillemoe, Cristina R. Ferrone
Massachusetts General Hospital, Boston, MA
Background: Advanced surgical techniques and new effective chemotherapeutic regimens have increased resection eligibility for colorectal liver metastases (CRLM), warranting reevaluation of prognostic factors. We sought to identify factors associated with overall (OS) and recurrence-free survival (RFS) in patients who underwent liver resection for CRLM in the modern era of treatment.
Methods: We identified 270 patients who underwent 292 curative liver resections for CRLM at our institution between 4/2000- 4/2014. All patients underwent resection of a primary colorectal cancer (CRC), and received contemporary systemic therapy with either Irinotecan and/or Oxaliplatin and 5-FU (FOLFOX, FOLFIRI). Clinicopathologic and treatment-related variables were evaluated for association with OS and RFS by multivariate analysis.
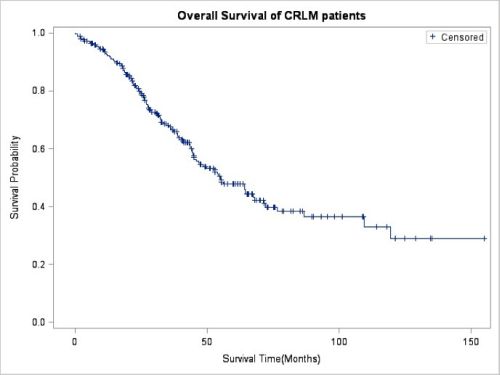
Results: The majority of patients were male (54%) with a median age at liver resection of 60 years (29-83). Median size of the largest metastasis was 25mm (1-150mm). Synchronous lesions were common (63%) and 40% had bilobar metastases. Most patients (79%) received neoadjuvant chemotherapy prior to liver resection. A Clavien complication with score >3 occurred in 53 patients (19%). 90-day mortality rate was 2% (6/270). Actuarial 5-year RFS and OS were 24% (95% CI: 19-30) and 48% (95% CI: 40-55) respectively. Significant prognostic factors for poor RFS were lymphovascular invasion (LVI) in the primary colorectal cancer (CRC) (p=0.001) and higher pre- liver resection CEA (p=0.003). Prognostic factors for poor OS were venous invasion in the primary CRC (p=0.024), size of the largest metastasis (p=0.021), and higher Clavien score (p=0.046). Chemotherapy after liver resection was significant for improved OS (p<0.001). Margin status, primary N stage, number and distribution of metastases were not significant (p>0.05).
Conclusion: In the era of FOLFOX and FOLFIRI, good surgical outcomes with low complication rates allowing for post-hepatectomy chemotherapy significantly improve OS. Pathologic factors representing the biology of the disease including LVI and venous invasion in the primary, size of the metastasis, and CEA level negatively affect OS.
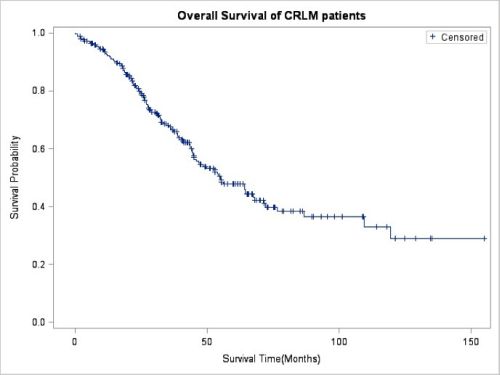
Fig. 1: Kaplan - Meier plot of overall survival for patient cohort
Back to 2015 Annual Meeting Program
|