|
Back to 2015 Annual Meeting Program
Robotic Colorectal Surgery: Does It Really Make a Difference?
Bradley J. Hensley*, Christian P. Probst, Christopher T. Aquina, Adan Z. Becerra, Katia Noyes, John R. Monson, Fergal Fleming
Surgery, University of Rochester Medical Center, Rochester, NY
Purpose:
Most colorectal resections are performed utilizing a laparoscopic or open approach. Over the past decade the number of robotic surgeries has increased as many surgeons believe it leads to better patient outcomes as compared to a laparoscopic approach. Therefore, it is imperative to clarify the benefits of robotic surgery as it is a costly technology. This study examines the relationship between laparoscopic, robotic and open operative approaches with post-operative complications following colorectal resection.
Methods:
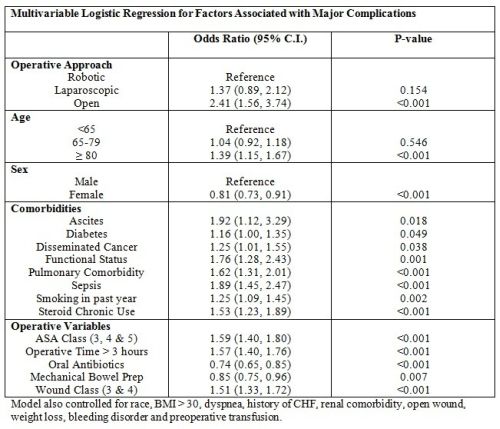
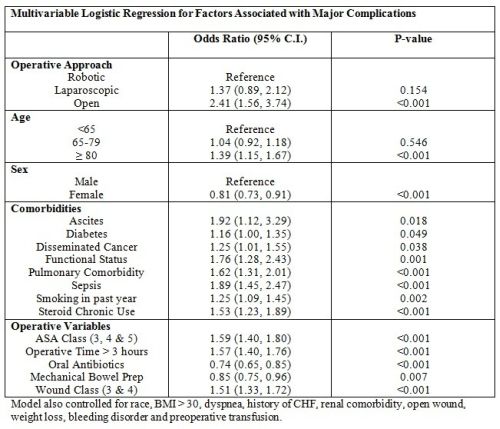
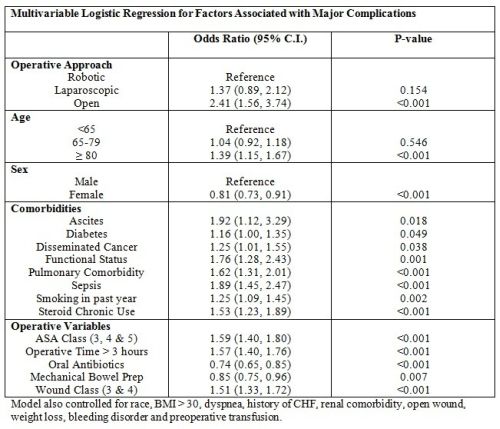
The 2012-2013 colectomy procedure targeted American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) database was queried for patients undergoing laparoscopic, open or robotic partial colectomy or low anterior resection using CPT codes 44140, 44145, 44204, and 44207. Emergent cases were excluded. Postoperative complications examined were incisional surgical site infections (superficial or deep SSI) and major complications. Major complications included the following organ system complications: respiratory (pneumonia, reintubation, or failure to wean from ventilator), cardiac (cardiac arrest requiring CPR, myocardial infarction), renal failure (acute or progressive renal failure), venous thromboembolic event (deep venous thrombosis or pulmonary embolism), sepsis or septic shock, organ space infection, anastomotic leak, neurological (coma >24 h, stroke/cerebrovascular accident), or major postoperative blood transfusion (>4 units of packed red blood cells given in the 72 h after surgery). Bivariate analysis compared complication rates across patient and surgical characteristics, and factors with a p-value <0.1 were included in multivariable analysis. Separate logistic regression models estimated the odds of each complication associated with laparoscopic, robotic and open operative approaches.
Results:
Of the 20,310 colectomy procedures 68.6% were laparoscopic, 29.1% were open and 2.3% were robotic. Overall 1,385 (6.8%) developed a SSI and 2,039 (10.0%) had a major complication. After adjusting for potential confounders, patients undergoing an open approach were 1.85 times more likely to experience an SSI (95% CI 1.15-3.00, p=0.012) and 2.41 times more likely to have a major complication (95% CI 1.56-3.74, p<0.001) than robotic surgery. Of note, there was no statistical difference in complication rates between laparoscopic and robotic surgeries (Table 1 and 2).
Conclusions:
While robotic surgery may yield better outcomes over open surgery and provide intraoperative benefits for the surgeon, this study does not provide evidence that robotic surgery is superior to laparoscopic surgery when it comes to complications. Further study is needed as the use of robotic surgery increases.
Back to 2015 Annual Meeting Program
|