|
Back to 2015 Annual Meeting Program
Evaluation of Completion Rate of ‘Upfront Surgery and Adjuvant Chemotherapy' According to Resectable Status of Pancreatic Head Cancers
Satoshi Nara*, Kazuaki Shimada, Minoru Esaki, Yoji Kishi, Hironobu Suto, Tomoo Kosuge
Hepatobiliary and Pancreatic Surgery Division, National Cancer Center Hospital, Tokyo, Japan
Background: Borderline resectable pancreatic ductal adenocarcinoma (PDAC) is associated with high rate of R1 resection and early postoperative recurrence. Although ‘upfront surgery and adjuvant chemotherapy' is established as a standard treatment for resectable PDAC, its efficacy may differ according to the resectable status assessed by preoperative images.
Patients and method: The consecutive 263 patients with a PDAC in the pancreas head who underwent laparotomy with an intent of curative pancreaticoduodenectomy at our hospital between 2005 and 2013 were analyzed in this study. All the patients underwent preoperative multidetector-row computed tomography (MDCT) examination. MDCT images of each patient were retrospectively reviewed and PDACs were classified into the following 3 groups. A: borderline resectable according to the NCCN guideline 2014, i.e. abutting to the superior mesenteric artery (SMA) less than 180 degrees, abutting to the common hepatic artery (CHA) with resection and reconstruction feasible or portal vein (PV) invasion over 180 degrees amenable to reconstruction, B: not abutting to the SMA or CHA but with suspected nerve plexus invasion around the SMA or the CHA, or PV invasion of less than 180 degrees, C: Others. None of the patients underwent neoadjuvant treatment, adjuvant radiation or laparoscopic staging laparotomy. The completion rate of adjuvant chemotherapy (AC) since 2008 was also assessed when AC has become a routine practice at our hospital.
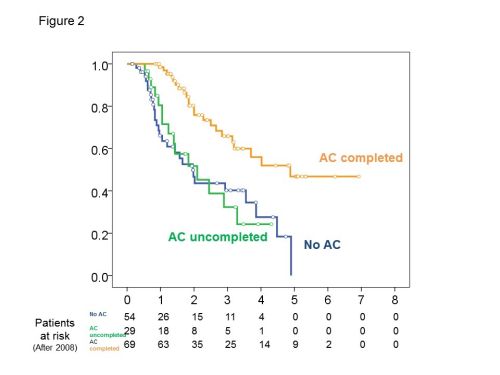
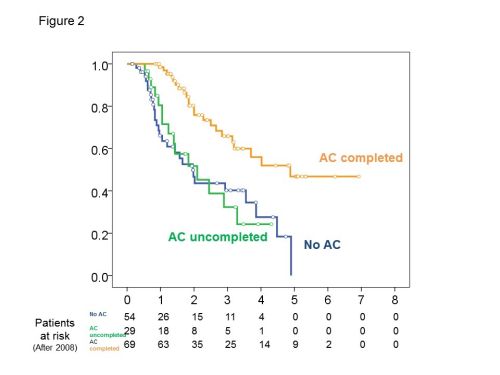
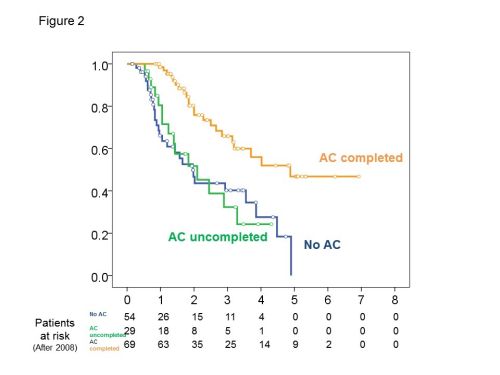
Results: The group A, B and C consisted of 51, 99 and 113 patients respectively. PDACs were unresectable at laparotomy due to distant metastasis or excessive local extension in 17, 10 and 13 patients in group A, B and C respectively. Among patients who underwent PD, R1 resection rates were 68%, 43% and 17%, median survival time (MST) was 12, 24 and 39 months (P<0.001, Fig 1) and the completion rates of AC were 21%, 48% and 52% in group A, B and C respectively. Patients who underwent R0 resection and completed AC were only 4% in group A. The major reasons for AC incompletion were poor physical condition in 24% and early recurrence in 47%. Two year overall survival rates of patients with no AC, uncompleted AC and completed AC were 47%, 52% and 78% respectively (P<0.001, Fig 2). Recurrences at peritoneal dissemination, but not in other sites were significantly increased in group A compared with group B or C (P=0.024).
Conclusion: In group A, the completion rate of ‘upfront surgery and adjuvant chemotherapy' was low. Neoadjuvant therapy seems to be suitable for group A. In group B, R1 resection rate was high, therefore AC is crucially important for them. In group C, R0 resection was achieved in 83% but the completion rate of AC was only 51%. Clinical trials seeking for a more feasible and effective adjuvant therapy, including neoadjuvant therapy is imperative in both group B and C.
Back to 2015 Annual Meeting Program
|