|
Back to 2015 Annual Meeting Program
Pancreaticoduodenectomy for Pancreatic Neuroendocrine Tumors: Are Combined Procedures Justified?
Cornelius a. Thiels*, Kristopher P. Croome, Danuel V. Laan, John R. Bergquist, Mark J. Truty
Surgery, Mayo Clinic, Rochester, MN
INTRODUCTION: The efficacy and outcomes of pancreatic resection for pancreatic neuroendocrine tumors (PNET) are well established. Few data exist looking specifically at pancreaticoduodenectomy (PD) alone for PNET. We aimed to clarify the outcomes of patients with PNET undergoing PD alone or with combined procedures.
METHODS: A retrospective review of all PD's performed from 1998 to 2014 at a single institution was conducted. Only pathologically confirmed PNET were included in the study. Patients were categorized into either standard PD (SPD) or combined PD (CPD) with CPD defined as those patients undergoing concurrent vascular reconstruction and/or additional organ resection in order to achieve complete tumor removal. Patient demographics, procedural and pathological data, and perioperative and long-term survival outcomes were collected. Kaplan-Meier curves were used to assess survival.
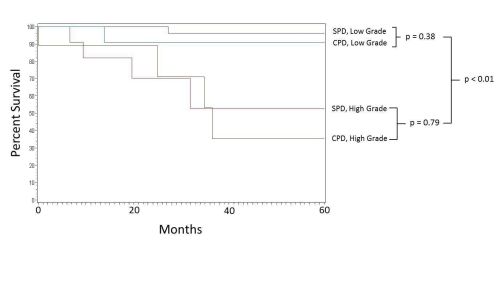
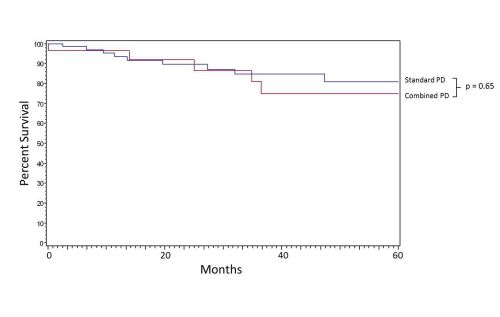
RESULTS: We identified 107 patients who underwent PD for PNET. Median patient age was 57 years. Thirty patients underwent CPD. This included 10 patients who underwent vascular resection and reconstruction, 21 patients underwent additional organ resection for either synchronous metastasis or adjacent locoregional tumoral involvement, and one patient with both. The 90-day perioperative mortality was 1.47% and 3.45% for SPD and CPD, respectively (p = 0.51). Median follow-up was 37 months. The overall 5-year survival after PD for PNET was 80.9% and 74.8% respectively; this was comparable between groups (p=0.65)(Figure 1). Overall 5-year survival was 94.9% for low-grade PNET vs. 43.4% for high-grade PNET undergoing PD (p<0.01) with grade, not extent of resection, being associated with worse postoperative survival (Figure 2).
CONCLUSION: Combination PD with vascular reconstruction and/or additional organ resection for PNET appears justified, particularly for patients with low-grade tumors. Tumor grade, rather than extent of resection, is associated long-term survival outcomes. The need for combinatorial procedures during PD is not a contraindication alone for otherwise resectable patients with PNET.
Figure 1. Kaplan-Meier survival curves of SPD and CPD showing equivalent survival at 60 months.
Figure 1. Kaplan-Meier survival curves of SPD and CPD showing equivalent survival at 60 months.
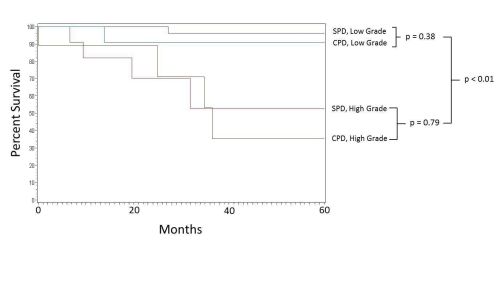
Figure 2. Kaplan-Meier survival curves of PD for PNET by tumor grade showing worse survival at 60 months in high grade tumors.
Back to 2015 Annual Meeting Program
|