|
Back to 2015 Annual Meeting Program
ERCP in Potentially Resectable Malignant Biliary Obstruction Remains Common and Is Associated With Frequent Failed Procedures When Performed Outside of an Academic Medical Center
Erica Donnan*1, David J. Bentrem2, Srinadh Komanduri3, Rajesh N. Keswani3
1Department of Medicine, Northwestern University, Chicago, IL; 2Department of Surgery, Northwestern University, Chicago, IL; 3Division of Gastroenterology, Northwestern University, Chicago, IL
Introduction:
There is Level 1 evidence that biliary decompression prior to pancreaticoduodenectomy (Whipple) is not necessary for most patients. When performed, it should be combined with endoscopic ultrasound (EUS) and potentially with metal stent placement to reduce the risk of early stent occlusion. It is unclear whether clinical practice is consistent with current evidence. The aim of this study is to examine endoscopic practice patterns and impact of center type upon initial management of patients with potentially resectable malignant biliary obstruction.
Methods:
This was a retrospective analysis of patients, identified using existing prospective surgical and endoscopic databases, presenting to our academic medical center (AMC) for endoscopic and surgical management of distal biliary obstruction due to suspected malignancy over a 3.5-year period (1/2011-6/2014). Patients with metastatic disease or >180 degree arterial involvement on pre-endoscopic cross-sectional imaging were considered unresectable at baseline and excluded. The analysis was stratified by whether patients underwent initial endoscopic management at a community medical center (CMC) or initial endoscopic/surgical management at the AMC.
Results:
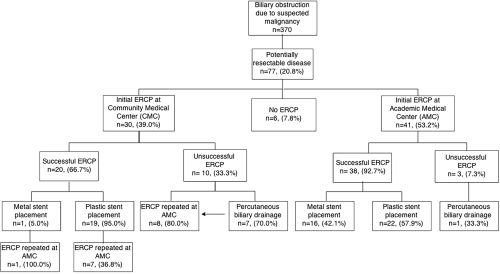
Of 370 patients identified with distal biliary obstruction due to suspected malignancy, 20.8% (n=77) presented with potentially resectable disease and were included for analysis. The majority (n=63, 82%) initially presented to a CMC. Of these 63 patients, 49% (n=31) underwent endoscopy at a CMC; the remaining patients (n=46) initially presented or were referred to our AMC for initial management (Figure).
ERCP was attempted in 92% of patients overall (Table). Biliary stent placement during ERCP was more successful at initial attempt at the AMC versus a CMC (93% vs. 67%, p=0.01) and the need to perform percutaneous biliary drainage less common at the AMC (2.4% vs. 23.3%, p=0.01). Of the 10 CMC ERCP failures, 7/8 had successful repeat ERCPs at the AMC. Metal stents were more commonly used during initial ERCP at the AMC (42% vs. 5%, p=0.002). The majority (81%) of patients who had an endoscopic work-up at a CMC required repeat endoscopy at the AMC for EUS+/-FNA (n=25) and/or ERCP (n=16). In total, 72 patients (96%) were diagnosed with pancreatic adenocarcinoma; 57% of all patients (n=44) underwent pancreaticoduodenectomy and the frequency did not differ by practice setting.
Conclusions:
Despite evidence that biliary decompression is not necessary in potentially resectable malignant distal bile duct obstruction, it remains common. Furthermore, when attempted biliary decompression occurs outside of an AMC, it is often unsuccessful and the majority of patients require additional endoscopy at an AMC for EUS or repeat ERCP. Further education is needed to limit the performance of unnecessary ERCP in this patient population.
Table. Management Based on Initial Treatment at Community Medical Center (CMC) versus Academic Medical Center (AMC)
| Initial Endoscopic Management at CMC (n=31) | Initial Endoscopic or Surgical Management at AMC (n=46) | Overall (n=77) | | ERCP Attempted | 30 (96.8%) | 41 (89.1%) | 71 (92.2%) | | Initial ERCP Successful | 20/30 (66.7%)* | 38/41 (92.7%) | 58/71 (81.7%) | | ERCP Complication within 72 hours | 4/30 (13.3%) | 1/41 (2.4%) | 5/71 (7.0%) | | Percutaneous Biliary Drain Placed After Unsuccessful ERCP | 7/30 (23.3%)* | 1/41 (2.4%) | 8/71 (11.3%) | | Metal Stent in Successful Initial ERCP | 1/20 (5.0%)** | 16/38 (42.1%) | 17/58 (29.3%) | | EUS Performed | 4 (12.9%)*** | 46 (100%) | 50 (64.9%) | | Underwent pancreaticoduodenectomy | 18 (58.1%) | 26 (56.5%) | 44 (57.1%) |
* P=0.01; **P=0.002; *** P<0.0001 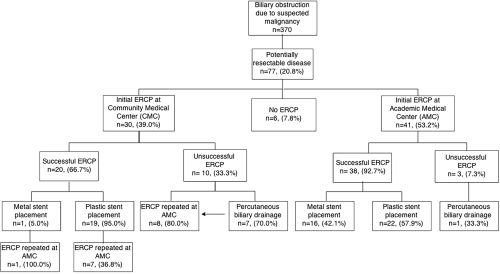 Initial Endoscopic Management at Community Medical Center (CMC) versus Academic Medical Center (AMC) Initial Endoscopic Management at Community Medical Center (CMC) versus Academic Medical Center (AMC)
Back to 2015 Annual Meeting Program
|