|
Back to 2015 Annual Meeting Program
Preoperative Esophageal Manometry Does Not Alter Operative Approach or Post-Operative Dysphagia Following Laparoscopic Paraesophageal Hernia Repair
Edward L. Jones*, Sara E. Martin Del Campo, Sara Mansfield, Kyle a. Perry
Surgery, The Ohio State University, Columbus, OH
Introduction: Laparoscopic paraesophageal hernia (PEH) repair typically involves creation of a complete or partial fundoplication. Some authors advocate for routine preoperative manometry to aid in surgical planning and reduce the likelihood of postoperative dysphagia. However, esophageal manometry can be difficult to perform in patients with large hernias and is associated with significant discomfort. We hypothesized that the use of routine preoperative manometry in patients with PEHs would not change the type of fundoplication performed or reduce postoperative dysphagia.
Methods and Procedures: We performed a retrospective review of all patients undergoing PEH repair between January 2011 and July 2014. Demographic, preoperative, operative, and outcome data were collected prospectively and maintained in an IRB approved database. The primary outcome measures included the type of fundoplication performed and post-operative dysphagia scores. Secondary outcomes included disease specific quality of life scores (GERD-HRQL) and patient satisfaction. Data were analyzed using Stata 12 software (Stata Corporation, College Station, TX) with significance set at p < 0.05.
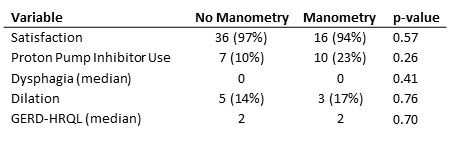
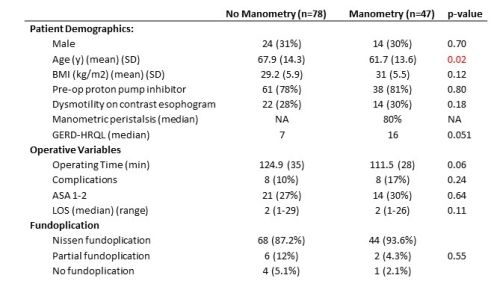
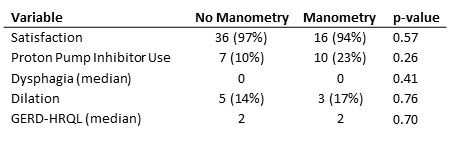
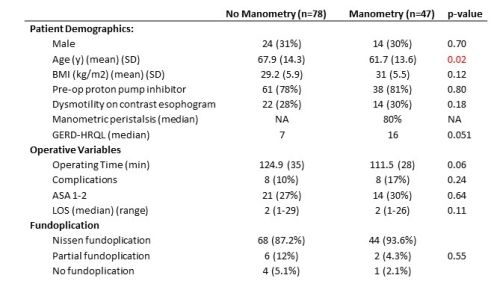
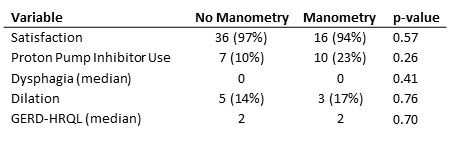
Results: One hundred twenty-five patients underwent laparoscopic PEH repair during the study period. Forty-seven (37%) patients underwent preoperative manometry, and 78 (62%) did not. The mean age was 65.6±14.3 years and 87 (70%) were female with a mean body mass index (BMI) of 29.9±5.8 kg/m2. Patients who did not undergo manometry were older (67.9 vs. 61.7, p=0.02), but the groups did not differ in terms of BMI, gender, Proton Pump Inhibitor (PPI) use, baseline dysphagia score, baseline GERD-HRQL score or type of fundoplication performed. At a median follow-up of 16 months (range 4 - 44 months), the median dysphagia score was 0 for both groups (p=0.41). Five (14%) patients in the no manometry group required endoscopic dilation compared to 3 (17%) in the manometry group (p=0.76). Median GERD-HRQL score improved significantly in both the no manometry and manometry groups (7 vs. 2, p<0.01 and 16 vs. 2, p<0.01 respectively). Overall 96% of patients were satisfied with their operation and 96% would choose to have surgery again given the benefit of hindsight.
Conclusions: Laparoscopic paraesophageal hernia repair with complete fundoplication is a safe and effective treatment that improves disease specific quality of life with a low rate of post-operative dysphagia. The use of preoperative manometry does not impact the choice of fundoplication and its omission does not increase the rate of post-operative dysphagia or the need for post-operative dilation. Hence, the routine use of preoperative manometry for patients undergoing paraesophageal hernia repair is not necessary. Further study is needed to define which patients may benefit from selective preoperative manometry.
Back to 2015 Annual Meeting Program
|