|
 |
Back to 2015 Annual Meeting Program
Overall Survival but Not Recurrence Is Impacted by Post-Operative Infection After Minimally Invasive Esophagectomy for Esophagogastric Adenocarcinoma
Vernissia Tam*2, James D. Luketich1, Inderpal S. Sarkaria1, Ryan Levy1, Neil a. Christie1, Omar Awais1, Manisha Shende1, Katie S. Nason1
1Cardiothoracic Surgery, University of Pittsburgh, Pittsburgh, PA; 2General Surgery, University of Pittsburgh, Pittsburgh, PA
Background:
Recent studies suggest that infectious complications after colorectal surgery compromise patient immunity and promote tumor recurrence, leading to worse survival. The impact of such complications on tumor recurrence and survival after esophagectomy for esophageal cancer, however, is unknown. Our study aimed to determine whether post-operative infection was associated with differences in tumor recurrence rate and overall survival following minimally invasive esophagectomy for esophageal adenocarcinoma.
Methods:
Patients who underwent minimally invasive esophagectomy for esophageal adenocarcinoma (n=825; 1997-2011) were stratified into two groups based on the presence or absence of at least one postoperative infectious complication (pancreatitis, Clostridium Difficile or urinary tract infection, wound infection/cellulitis, sepsis, anastomotic leak, gastric conduit leak, or pulmonary infection [pneumonia, empyema]). Kaplan-Meier curves for the primary outcomes of overall survival and time to tumor recurrence were compared using log-rank test. Cox regression and multivariable logistic regression were used to analyze factors associated with survival, time to recurrence and post-operative infection.
Results:
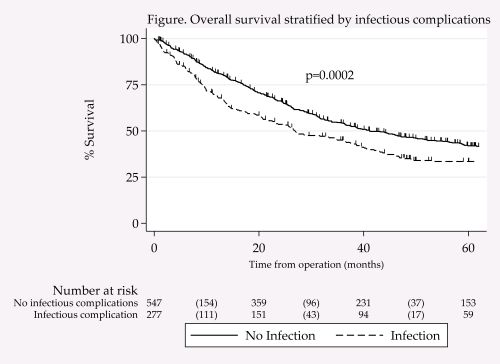
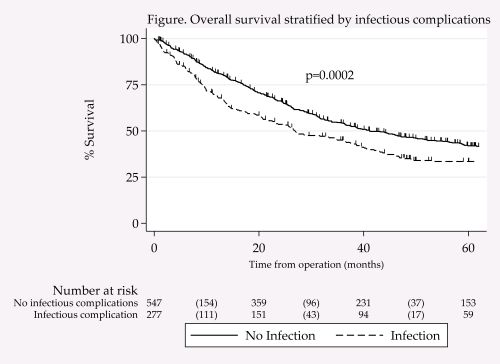
Infectious complications, identified in 34% of patients (n=277/825), were more likely in older patients with more comorbid diseases and higher age-adjusted Charlson Comorbidity Index score. Recurrent disease was identified during follow up in 38% (n=310); there was no association between infectious complications and the rate of or time to recurrence (p=0.28 and 0.39, respectively). At a median follow-up of 29 months, 64% of patients were dead. Greater long-term survival was found for patients who did not experience post-operative infectious complications (median 32 mo vs. 23 mo; p=0.0002). After adjusting for age, Charlson score, R0-resection status, neoadjuvant therapy and pathologic stage, infectious complications were independently predictive of increased hazard for death (HR 1.4; 95% CI 1.2-1.7).
Conclusions:
Consistent with reported rates after esophagectomy, infectious complications were identified in 34% of patients, who tended to be older and have more comorbid disease. Contrary to the colorectal data, the presence of post-operative complications was not associated with increased rate of recurrence. We did, however, find that infectious complications were independently associated with worse overall survival. These data emphasize the need for ongoing efforts to identify patients at risk and optimize postoperative strategies to reduce the incidence of postoperative infections.
Back to 2015 Annual Meeting Program
|