|
Back to 2015 Annual Meeting Program
Modified Appleby Procedure With Arterial Reconstruction: a Literature Review and Report of 3 Unusual Cases
Jessica a. Latona*1, Kathleen M. Lamb1, Daniel Relles2, 1, Warren R. Maley1, Charles J. Yeo1
1Surgery, Thomas Jefferson University Hospital, Philadelphia, PA; 2Pediatric Surgery, Morgan Stanley Children's Hospital, New York, NY
BACKGROUND
Pancreatic body and tail carcinomas are often diagnosed with local vascular invasion of the celiac axis (CA) and its branches. With such involvement, these tumors have traditionally been considered unresectable. The modified Appleby procedure allows margin negative resection of such locally advanced tumors. This procedure involves distal pancreatectomy with en bloc splenectomy and CA resection and relies on the presence of collateral arterial circulation via an intact pancreaticoduodenal arcade and gastroduodenal artery (GDA). When the resultant collateral circulation is inadequate to provide sufficient hepatic and gastric arterial inflow, arterial reconstruction (AR) is necessary to "supercharge" the inflow. Herein, we review all reported cases of AR with modified Appleby procedures and report our experience of 3 recent cases with arterial reconstruction including 2 cases with arterial bypasses not requiring interposition grafting.
METHODS
A PubMed search was systematically completed of studies relating to distal pancreatectomy with CA resection and subsequent AR.
RESULTS
Eleven reports involving 27 patients were identified of distal and total pancreatectomy with AR after CA resection (Table 1). The most common AR, performed in 11 patients, was a bypass from the aorta to the common hepatic artery (CHA) using a variety of interposition conduits. In our experience, patient #1 had a primary side to end aorto-CHA bypass, patient #2 had a primary end to end bypass of the distal CHA to the left gastric artery (LGA) in the setting a replaced left hepatic artery (rLHA), and patient #3 required an aortic to proper hepatic artery bypass with saphenous vein graft and venous reconstruction. Patient #1 received adjuvant chemo-radiation therapy. Patient #2 received neoadjuvant chemotherapy and proton therapy with a near complete tumor response. Patient #3 received neoadjuvant chemo-radiation therapy with a near complete tumor response. All patients recovered well and they are currently 6, 5 and 2 months post-op, respectively.
CONCLUSIONS
Criteria for resectablilty in patients with locally advanced pancreatic body and tail neoplasms are expanding due to increasing experience with AR in the setting of the modified Appleby procedure. When performing AR, primary anastomosis may be considered preferable to interposition grafting as it decreases the potential for the infectious and thrombotic complications associated with conduits and it reduces the number of vascular anastomoses from two to one. Consideration must also be given to normal variant anatomy of the hepatic circulation (as seen in patient #2) during operative planning as the LGA is resected with the CA. The modified Appleby with AR, when used in appropriately selected patients, offers the potential for safe, margin negative resection of locally advanced tumors.
Table 1: Reported cases of Vascular Reconstruction During Modified Appleby Procedure
| Arterial reconstruction (AR) | Conduit | | Konishi (2000) | CA to CHA (n=2) | SA | | Miyakawa (2002) | CA to CHA | IMV | | Kondo (2003) | Left MCA branch to GEA (n=2) | primary micro | | Gagandeep (2006) | CA to LGA | primary | | Machado (2009) | Left EIA to HA | Dacron (8mm) | | Wu (2009) | CA to CHA (n=4) | pimary, SA, IMV or RGSV | | Bockhorn (2011) | Ao/SMA to PHA, Aberrant LHA to PHA (total n=5) | Cryo-vein, RSVG (total n=5) | | Baumgartner (2012) | Ao to CHA | Unspecified vein | | Ielpo (2013) | Ao to CHA | Dacron (8mm) | | Suzuki (2012) | PHA to MCA | primary | | Christians (2013) | CA to CHA (n=3) | RSVG (n=3) | | 3 case series (2014) | Ao to CHA (n=1), Distal CHA to LGA (with rLHA) (n=1), Ao to PHA (n=1) | primary (n=2), RSVG (n=1) |
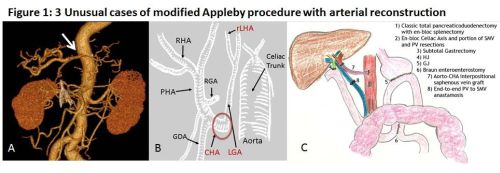
CA = celiac axis; CHA = common hepatic artery; SA = splenic artery; IMV = inferior mesenteric vein; MCA = middle colic artery; GEA = gastroepiploic artery; LGA = left gastric artery; EIA = external iliac artery; HA = hepatic artery; RSVG = reversed saphenous vein graft; Ao = aorta; PHA = proper hepatic artery; rLHA = replaced LHA; micro = microsurgical 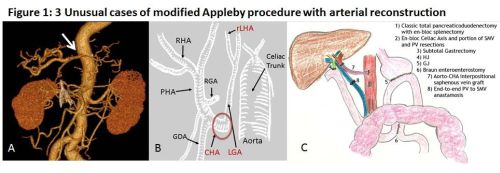 A. Postoperative three-dimensional computed tomography angiogram of patient #1 showing the patency of the primary aortic to common hepatic artery bypass (arrow). B. Schematic representation of the postoperative arterial reconstruction of patient #2 showing a primary end to end bypass of the distal common hepatic artery (CHA) to the left gastric artery (LGA) in the setting of a replaced left hepatic artery (rLHA). C. Schematic representation of the postoperative anatomy of patient #3 showing classic total pancreatectomy with en bloc splenectomy, celiac axis and SMV-Portal vein resection followed by subtotal gastrectomy, aortic to CHA bypass with RSVG (7) and primary PV to SMV reconstruction (8).
Back to 2015 Annual Meeting Program
|