|
Back to 2015 Annual Meeting Program
Does the Pancreatic Resection Have Any Survival Benefit in Patients With a Pancreatic Adenocarcinoma and Intraoperatively Diagnosed Positive Para-Aortic Lymph Node Metastasis or Peritoneal Lavage Cytology?
Hironobu Suto*, Satoshi Nara, Yoji Kishi, Minoru Esaki, Kazuaki Shimada, Tomoo Kosuge
National Cancer Center Hospital, Tokyo, Japan
Background. The positive para-aortic lymph node metastasis (PA+) or peritoneal lavage cytology (CY+) in patients with resectable pancreatic ductal adenocarcinoma is associated with poor prognosis. However, some patients may benefit from tumor resection compared with no resection.
Method. Seven hundred eleven patients who underwent laparotomy for invasive ductal adenocarcinoma of the pancreas with intent of curative resection from 2001 to 2013 at our hospital were included in this study. All the patients underwent preoperative contrast-enhanced computed tomography (CT) and ultrasonography examinations and had no apparent sign of PA+ or distant metastases. All the patients underwent routine intraoperative peritoneal lavage cytology and frozen section analysis of PA. The patients were divided into the following 4 groups: A: not resected due to intraoperatively discovered liver metastasis (H+) or peritoneal dissemination (P+), B: not resected due to PA+, CY+, or locally advanced cancer (H-, P-), C: resected despite of PA+ or CY+ (H-, P-), D: resected with PA-, CY-, H-, P-. Group C were further divided into C1: PA+ alone and C2: CY+ alone and C3: PA+ and CY+. Clinicopathological data and survival were compared among the 4 groups and multivariate analysis was performed to find prognostic factors.
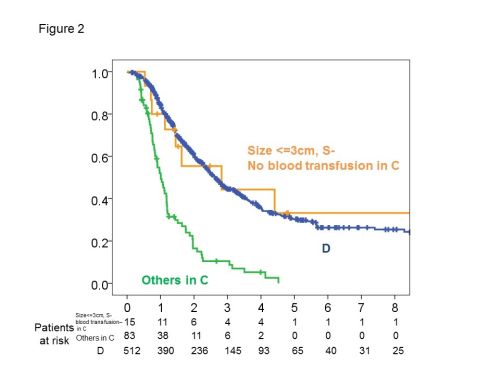
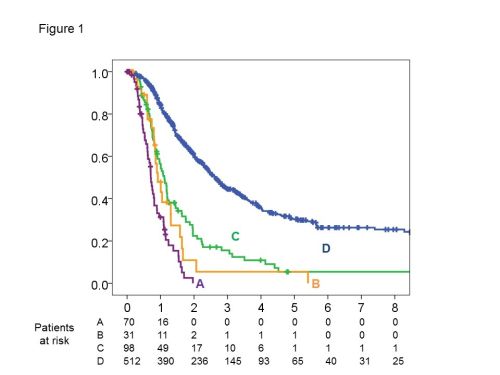
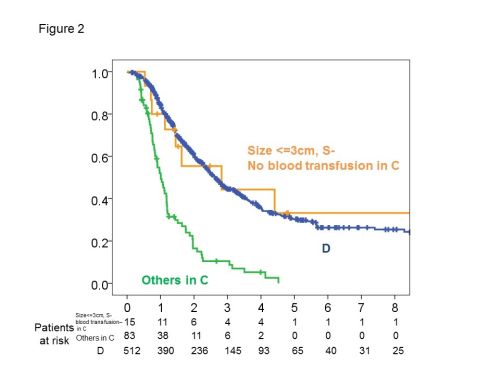
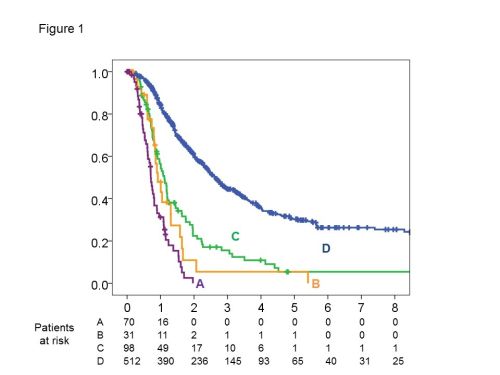
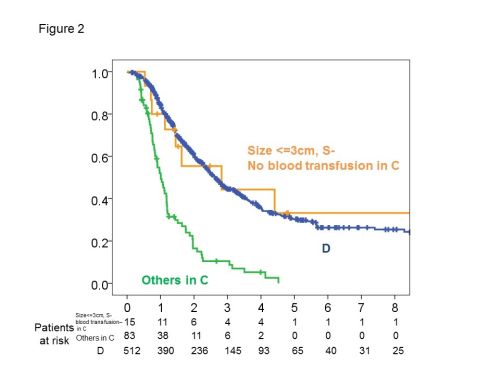
Results. Group A, B, C and D were composed of 70 (10%), 31 (4%), 98 (14%) (C1: 45, C2: 42, C3: 11) and 512 (72%) patients. There was no significant difference in overall survival (OS) between C1 and C2 (P=0.260). The 2-year OS and median survival time (MST) of each group (A, B, C and D) were 0, 10.9, 22.4 and 60.8%, and 8.5, 11.0, 13.3 and 31.7months (C vs A: P<0.001, C vs D: P<0.001, C vs B: P=0.288, Figure 1). The 1-year disease-free survival (DFS) and median DFS of group C were 16.5% and 5.6 months. Ten of 98 patients in group C survived more than 3 years. Univariate analysis revealed that tumor size >3cm, serosal invasion (S+), intraoperative blood transfusion, CA19-9>1000 U/mL and (CY+ and PA+) were significant poor prognostic factors in group C. In multivariate analysis, tumor size >3cm, S+ and intraoperative blood transfusion were independent poor prognostic factors. The 3-year OS of 15 patients in group C with tumor size <=3cm, S- and no blood transfusion was 44%, which was better than 10% in others of group C (P=0.001) and similar to 45% in group D (P=0.936, Figure 2).
Conclusion. No resection is appropriate in most of the patients in group C because of high likelihood of early recurrence and poor prognosis after resection. This emphasizes the importance of intraoperative pathological diagnosis. But some patients in group C with tumor sized less than 3cm, S- and no requirement of blood transfusion may benefit from resection with a similar survival to group D.
Back to 2015 Annual Meeting Program
|