|
Back to 2015 Annual Meeting Program
Malignant Progression in Intraductal Papillary Mucinous Neoplasms of the Pancreas: Outcome of Initially Selected for Resection or Primary Surveillance
Takuya Sakoda*, Yoshiaki Murakami, Kenichiro Uemura, Yasushi Hashimoto, Naru Kondo, Naoya Nakagawa, Kazuhide Urabe, Hayato Sasaki, Hiroki Ohge, Taijiro Sueda
Department of Surgery, Applied Life Sciences Institute of Biomedical & Health Sciences, Hiroshima University, Hiroshima, Japan
BACKGROUND: There is international consensus that most branch duct IPMNs (BD-IPMN) harbor a low risk of progression to malignancy and can be safely managed with observation alone. However, the natural history of patients undergoing primary surveillance is poorly understood and there is still ongoing controversy about surgical indication of BD-IPMN. This study describes the natural history of IPMN in patients initially selected for resection or primary surveillance with respect to risk factors of malignant transformation.
METHODS: All consecutive patients who underwent surgery for IPMN between April 1990 and August 2014 were included. Low versus high oncologic risk was stratified prospectively and compared with histopathological features.
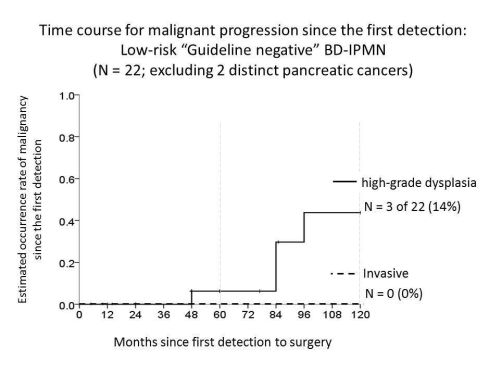
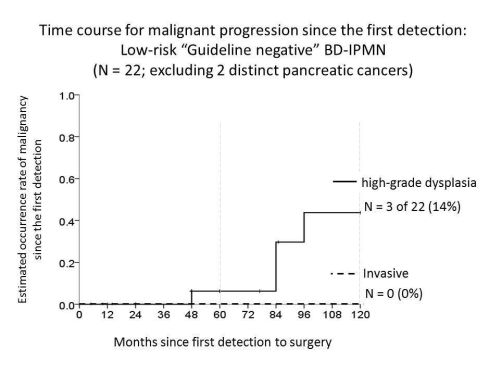
RESULTS: A total of 162 patients underwent pancreatic resection for IPMN. Based on the preoperative imaging, 38 (23%) patients had main duct involved IPMN, 56 (35%) had mixed-type, and 68 (42%) had suspected BD-IPMNs. Initial resection was selected for 131 patients (81%) and invasive disease was identified in 38% (50/131). Primary surveillance was selected for 31 patients (19%) and ultimately underwent resection: 6 mixed-type and 25 BD-IPMNs. Median follow-up for the primary surveillance was 5.5 years. Of the 31 patients for primary surveillance, 24 (77%) initially stratified as low-risk IPMN (guideline negative) developed a new indication for pancreatic resection: development of intramural nodule (n=22) and extension to main pancreatic duct (n=16), new onset of symptom (n=3), and invasive lesions developed in a region remote from the index IPMN (n=2). On histopathology, 18 patients had low-grade, 2 had intermediate-grade, 8 had high-grade dysplasia, and 3 had invasive disease associated with IPMN on histopathology. Overall, invasive disease was identified in 23% (7/31) for primary surveillance, of which 4 (13%) patients developed distinct invasive ductal adenocarcinomas in a region separate from the index cyst, representing 57% (4 of 7) with invasive disease during surveillance. Among the 24 patients initially determined to be low-risk (guideline negative), 5 patients developed high-grade dysplasia (4.0-10.4 years after initiating surveillance) and only one patient developed invasive cancer associated with IPMN over 10 years after initially diagnosed as BD-IPMN (10.5 yeas).
CONCLUSIONS: Progression to invasive cancer during primary surveillance for low-risk BD-IPMN was rare. Diagnostic, operative, and surveillance strategies for IPMN should consider increased risk not only to the index cyst but also the entire gland for developing distinct pancreatic cancer.
Back to 2015 Annual Meeting Program
|