|
 |
Back to 2015 Annual Meeting Program
Predicting the Need for Dependent Care in Geriatric Patients After Emergency Cholecystectomy
Yaser M. Baghdadi*1, Dan S. Ubl2, Asad J. Choudhry1, Cornelius a. Thiels1, Elizabeth B. Habermann2, Donald Jenkins1, Martin D. Zielinski1
1Department of Surgery, Division of Trauma, Critical Care and General Surgery, Mayo Clinic, Rochester, MN; 2Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery, Mayo Clinic, Rochester, MN
Introduction: There is great demand for dependent care (DC) facility placement for elderly emergency surgery patients at dismissal. To improve the efficiency of discharge planning, we aimed to identify preoperative risk factors for DC needs on dismissal.
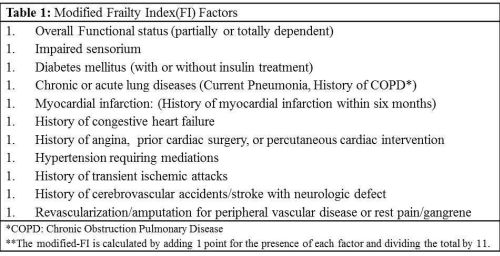
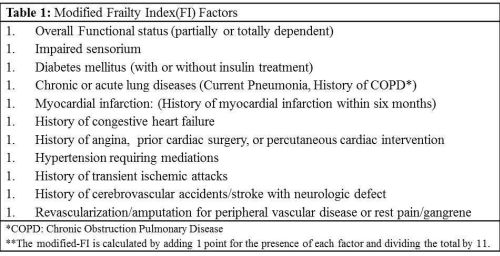
Methods: Patients 65 years or older who underwent emergency cholecystectomy were identified in the National Surgical Quality Improvement Program (NSQIP) database from 2011 to 2012. Patients who had an unknown discharge destination, in-hospital death, or were admitted from a DC facility, were excluded. Patient characteristics, complications, and discharge destinations were analyzed. The 11-factor-modified-frailty index (FI), derived from the Canadian Study of Health and Aging and validated in the ACS-NSQIP database, was used to categorize pre-existing factors associated with physiologic frailty and the likelihood of DC disposition (Table 1). Statistically significant univariate features (p<0.05) were incorporated into two multivariable logistic regression models; 1) the total number of modified- FI factors (as an ordinal variable), and 2), the modified-FI factors considered as individual components (i.e. binary variables) in order to define specific risk factors for DC care.
Results: Of the 1,430 patients, 241 (17%) were dismissed to a DC facility. In the first multivariable model, patients with zero (OR 0.25, 95% CI 0.14 - 0.45), one (OR 0.29, 95% CI 0.18 - 0.46), or two FI factors (OR 0.51, 95% CI 0.31 - 0.85) had statistically significantly decreased odds for DC placement after emergency cholecystectomy compared to patients with three or more factors. The second model identified impaired sensorium (OR 7.4, 95% CI 2.4 - 23.2), lung disease (OR 2.3, 95% CI 1.4 - 3.9), congestive heart failure (OR 2.8, 95% CI 1.1 - 6.9), hypertension requiring medications (OR 1.6, 95% CI 1.1 - 2.4), and partial/full assistance (OR 4.2, 95% CI 2.5 - 7.1), were statistically significant risk factors for discharge to a DC facility.
Conclusions: Discharge to a DC facility after emergency cholecystectomy was independently associated with multiple factors of the modified-FI. The modified-FI would be helpful in early planning for hospital dismissal among elderly surgery patients.
Back to 2015 Annual Meeting Program
|