|
 |
Back to 2015 Annual Meeting Program
Complete Pathologic Response Is an Independent Predictor of Improved Survival Following Neoadjuvant Chemoradiation for Esophageal Adenocarcinoma.
Raed M. Alnaji*1, William Du2, Smit Singla3, Kristopher Attwood4, Hector Nava3, Usha Malhotra3, Moshim Kukar3, Steven Hochwald3
1Department of Internal Medicine, University at Buffalo, Buffalo, NY; 2School of Medicine and Biomedical Sciences, University at Buffalo, Buffalo, NY; 3Department of Surgical Oncology, Roswell Park Cancer Institute, Buffalo, NY; 4Department of Biostatistics, Roswell Park Cancer Institute, Buffalo, NY
Introduction: Reports of improved survival in patients with complete pathologic response (cPR) to neoadjuvant therapy for esophageal and gastroesophageal junction (GEJ) adenocarcinoma is extrapolated from heterogeneous studies that include squamous cell histology. It is well known that squamous cell cancers are biologically different and respond better to chemoradiation. Therefore, we sought to determine if a complete pathologic response is associated with a survival advantage in a homogenous group of patients with esophageal and GEJ adenocarcinoma, undergoing multimodality treatment.
Methods: A single institution analysis of all patients with > or = T2 or node positive esophageal and GEJ (Siewert's Type 1 and 2) adenocarcinoma treated with neoadjuvant chemoradiotherapy and esophagectomy between 2004 and 2014 was conducted. Patients were divided into two groups based on pathological response {cPR vs incomplete pathological response (iPR)}. Patient and treatment characteristics were compared across groups using Wilcoxon rank sum and Fisher's exact tests. Survival outcomes were evaluated using standard Kaplan-Meier methods, with multivariate analyses utilizing Cox regression models.
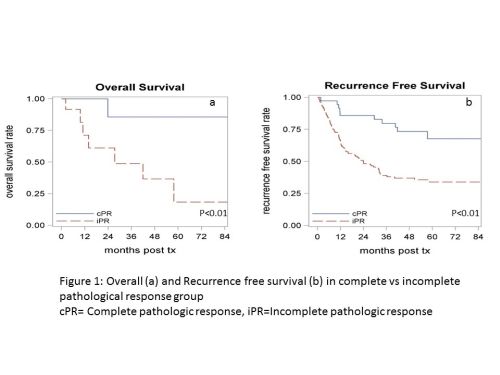
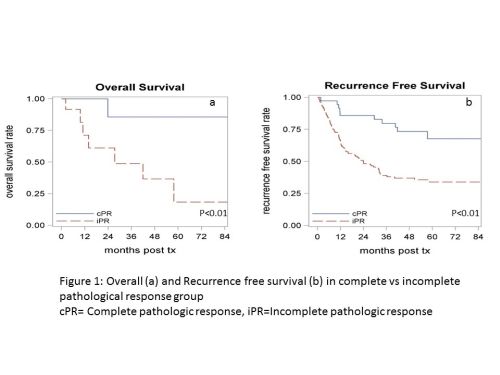
Results: 205 patients (M: 193, F: 12; median age, 61 years) were included in the study. 38 (19%) cPR patients were compared to 167 (81%) iPR patients. The 2 groups were similar with respect to clinical stage, age, gender, comorbid conditions, ECOG status, smoking and alcohol use. Patients in the cPR group had a higher percentage of tumors located in middle third of esophagus (11% vs 2%, p=0.04) while tumor grade was similar in both groups. Patients in the iPR group had a statistically higher incidence of pulmonary complications (31% VS 11%, p=0.009 and reoperation rate (18% vs 0%, p=0.002). Median follow up was 50 months (range 2 -109 months). 3 year overall and recurrence free survival for iPR was 48 months and 39 months vs 86 months and 80 months for cPR group, respectively (Figure 1a and 1b).
Conclusion: This analysis of a large cohort of homogeneous patients with esophageal and GEJ adenocarcinoma undergoing trimodality therapy highlights that complete pathologic response is an independent predictor of improved overall and recurrence free survival.
Back to 2015 Annual Meeting Program
|