|
Back to 2015 Annual Meeting Program
Quantitative Assessment of Esophageal Emptying in Achalasia Patients Using Esophageal Transit Scintigraphy
Joshua a. Boys*1, Daniel S. OH1, Jack Seto2, Robert W. Henderson2, Steven R. Demeester1, Jeffrey a. Hagen1
1Surgery, Univ. of Southern California, Los Angeles, CA; 2Nuclear Medicine, University of Southern California, Los Angeles, CA
Introduction: Timed barium studies using x-ray images 1 and 5 minutes following ingestion of liquid barium is currently the most common method to assess esophageal emptying before and after treatment in achalasia patients. However, interpretation of this study is relatively subjective and variable. An alternative technique of esophageal transit scintigraphy (ETS) was developed to assess esophageal clearance in a quantitative manner. We report the technical protocol that we have developed and its initial utilization in a cohort of achalasia patients before and after surgical myotomy.
Methods: Patients were prepared for the study by being NPO overnight. The entirety of the study was performed with the patient standing or sitting upright. The camera was centered to include the esophagus, stomach, and as much small bowel as possible. The patient was instructed to swallow 1.5mCi of technetium 99m sulfur colloid mixed in 30 cc of water followed immediately by an additional 120 cc of water for a total of 150 cc ingested. With the patient upright, 15 second static images were obtained at 0, 1, 5 and 10 minutes. Post scintigraphy analysis included outlining 2 regions of interest (ROI): ROI 1 over the esophagus and ROI 2 over the esophagus, stomach and as much small bowel as present in field of view. The percent of liquid remaining in the esophagus was calculated by dividing ROI1 by ROI2 with reporting of the percent remaining in the esophagus at time 0, 1, 5 and 10 minutes.
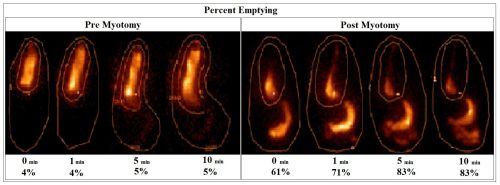
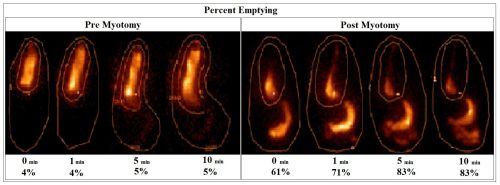
Results: There were 3 patients studied with the present protocol: 2 males and 1 female. All patients were diagnosed with achalasia and had a laparoscopic Heller myotomy with Dor fundoplication. The median percent emptying pre myotomy at 0, 1, 5, and 10 min was: 0% (0-4%), 4% (0-5%), 5% (0-10%), and 5% (0-10%). The median percent emptying post myotomy at 0, 1, 5, and 10 min was: 61% (29-76%), 77% (71-95), 85% (78-95%), and 83% (78-95%). Examples of ETS images with ROI outlines and percent emptying are shown in the figure.
Conclusion: We report a standardized technique of esophageal transit scintigraphy that allows quantitative assessment of esophageal clearance in patients with achalasia. By taking into account the amount of radioisotope that can immediately enter the stomach and small bowel with swallowing, it avoids the subjective nature of timed barium studies, particularly in the post-treatment setting. Future studies will be necessary to determine clearance percentages that correlate with symptom outcomes following treatment.
Back to 2015 Annual Meeting Program
|