|
Back to 2015 Annual Meeting Program
Extent of Lymph Node Involvement After Esophagectomy With Extended Lymphadenectomy for Esophageal Adenocarcinoma Predicts Recurrence: a Large North American Cohort Study
Sara Najmeh*, Henry Jiang, Mara L. Leimanis, Pedram Mossallanejad, Jonathan Cools-Lartigue
Surgery, McGill University, Montreal, QC, Canada
Background: Esophagectomy remains the cornerstone of curative treatment for esophageal adenocarcinoma, however recurrence remains high. Although previous studies have examined the rate of recurrence related to lymph node involvement, there is little data on these patterns after extended D2 lymphadenectomy for esophageal adenocarcinoma. We sought to identify patient, tumor and surgery-related factors associated with disease recurrence after en-bloc esophagectomy and extended lymphadenectomy for esophageal adenocarcinoma.
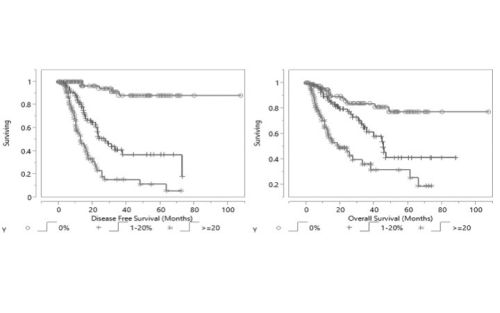
Methods: Patients undergoing complete resection of esophageal or EGJ adenocarcinoma from 2005-2014 in a university-affiliated North American hospital were identified from a prospectively collected database. Patient demographics, neoadjuvant treatment, OR and tumor characteristics, pathology outcomes, and follow up data were reviewed. Survival data was compared based on extent of lymph node involvement (absolute number and ratio). Chi-square test was used to test independence and colinearity within predictors of recurrence and survival. DFS and OS were analyzed using the Kaplan-Meier method, and the association of variables with time to recurrence and death was modeled using the Cox Proportional Hazards model. Student's t-test and Fisher's exact test were used to compare continuous and categorical variables, p <0.05 = *.
Results: A total of 216 patients who underwent curative resection for esophageal and EGJ cancers were identified. 123 patients (58%) received neoadjuvant chemotherapy and 168 patients (79.2%) underwent a D2 lymphadenectomy. The median total number of lymph nodes resected was 31[5-84] and median number of positive lymph nodes was 2[0-34]. 80 patients (37%) recurred at a median follow up of 13.6 months [1.5-72.7]; with 65 patients (81.25%) having distant recurrences vs 15 patients (18.75%) having locoregional recurrences. Having a positive lymph node number (+LN) >4 and a positive:total lymph node ratio (LNR)> 0.2 were associated with decreased overall and disease free survival. T stage>2, poor grade, lymphovascular invasion, perineural invasion, >4 positive LNs and LNR>0.2 were predictors of recurrence.
Conclusion: Higher number of positive lymph nodes and higher LNR were associated with lower overall and disease free survival in patients undergoing en bloc esophagectomy with D2 lymphadenectomy for esophageal adenocarcinoma. Irrespective of extent of LN involvement, the majority of recurrences were distant, implying efforts to improve outcomes should be directed towards enhancing systemic, rather than local, control.
Back to 2015 Annual Meeting Program
|