|
Back to 2015 Annual Meeting Program
Rural Disparities in Esophageal Cancer Outcomes Based on Distance From Endoscopic Ultrasound (EUS)-Trained Gastroenterologists
James Regan*1, Whitney Zahnd2, Bridget Kistner1, Aman Ali3, John D. Mellinger1, Sabha Ganai1
1Surgery, Southern Illinois University School of Medicine, Springfield, IL; 2Center for Clinical Research, Southern Illinois University School of Medicine, Springfield, IL; 3Gastroenterology, Southern Illinois University School of Medicine, Springfield, IL
Background: While centralization of esophagectomy has been advocated based on strong relationships of hospital and surgeon volume to mortality, rural disparities have not been explored for esophageal cancer outcomes. Opportunities are recognized for improvement in global systems related to esophageal cancer care including appropriate referral for surgical resection. This study explores the impact of rurality, gastroenterologist (GI) density and proximity to Endoscopic Ultrasound (EUS)-performing providers on outcomes for esophageal cancer in Illinois.
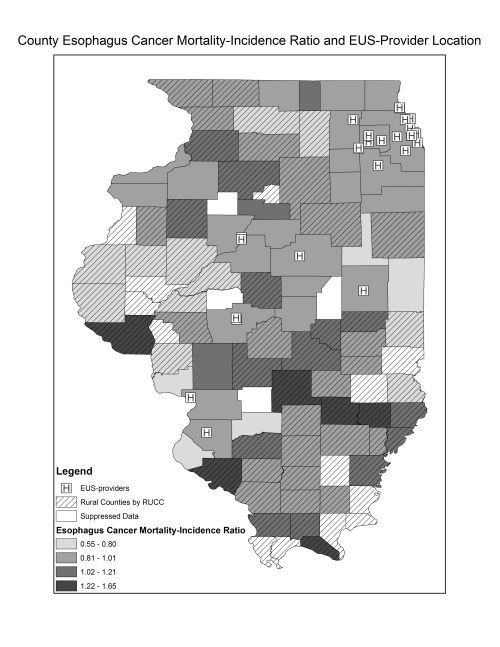
Methods: Age-adjusted esophageal cancer incidence rates were calculated for each county using 1991-2010 data from the Illinois State Cancer Registry. Age-adjusted mortality rates were calculated using SEER*STAT. Choropleth maps were created to illustrate Mortality-Incidence Ratios (MIRs) by Illinois county using ArcGIS. Mean GI density for each county was calculated from the US Area Health Resource File. Unique providers who perform EUS were identified and their locations geocoded for spatial analysis to calculate the shortest driving distance from each county centroid to the nearest EUS provider. USDA Economic Research Service rural-urban continuum codes (RUCC) and US census percent rurality data were used to designate county rurality and adjacency to metro counties. US Census Bureau county-based education, health insurance, income, and poverty data were used to determine socioeconomic deprivation levels.
Chi-square, t-test, ANOVA, and Spearman's rho calculations were performed.
Results: Access to GIs within a county was significantly influenced by county-level predictors including rurality, income, and educational status (p<0.05). No GIs were located in 65 out of 102 Illinois counties (64%) during the time interval analyzed, with a mean density of 1.0 per 100,000. There was a trend toward greater esophageal cancer incidence with increasing GI density (Spearman's rho=0.19; p=0.06). Median driving distance to the closest EUS provider was 28 miles in metro counties (n=36), 54 miles in rural counties adjacent to metro counties (n=33), and 98 miles in rural counties non-adjacent to metro counties (n=33; p<0.001). Distance to EUS-trained providers significantly correlated with both rurality and socioeconomic deprivation (p<0.001). Esophageal cancer MIR was positively correlated with RUCC (Spearman's rho=0.28; p=0.01) and EUS-provider distance (Spearman's rho=0.26; p=0.02).
Conclusions: Higher MIR for esophageal cancer was observed in rural regions and was correlated with distance from EUS-trained providers. Outcomes may be influenced by the availability of specialist gastroenterologists, which may be a surrogate for a higher level of care. Further exploration of the impact of distance from high volume cancer centers and surgeons on rural cancer outcomes is warranted.
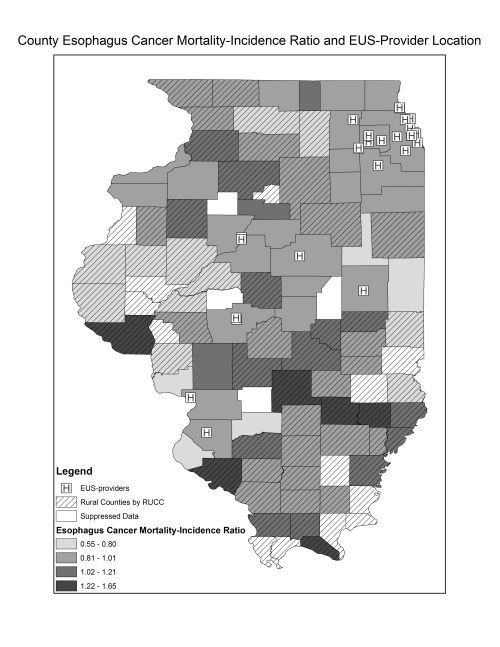
Choropleth map demonstrating Esophageal Cancer Mortality-Incidence Ratio (MIR) and Rurality by Illinois County. Unique providers with capabilities of performing Endoscopic Ultrasound (n=28) are designated as [H]. Twenty out of 23 (87%) Illinois counties with MIR greater than 1.02 were rural.
Back to 2015 Annual Meeting Program
|