|
 |
Back to 2015 Annual Meeting Program
No Heterogeneity of Treatment Effect Based on Hospital Volume in Gastric Cancer Patients Undergoing Surgery: All Patients Should Be Treated At High Volume Centers
Cristina Harnsberger*1, Hans F. Fuchs1, 2, Ryan C. Broderick1, Garth R. Jacobsen1, Bryan J. Sandler1, David C. Chang3, Santiago Horgan1, Kaitlyn J. Kelly1
1Surgery, University of California, San Diego, San Diego, CA; 2Surgery, University of Cologne, Cologne, Germany; 3Surgery, Massachusetts General Hospital, Harvard Medical School, Codman Center, Boston, MA
INTRODUCTION:
High hospital volume has a protective effect on surgical outcomes, however, it is not known whether the effect is different depending on the patient population studied. We sought to analyze the treatment effect with regard to in-hospital mortality in different patient populations who undergo gastric resection for cancer, based on hospital volume.
METHODS AND PROCEDURES:
The Nationwide Inpatient Sample (NIS) database was used and data was extracted using ICD-9 codes. Adults were included if they had a diagnosis of gastric cancer and underwent a potentially curative partial or total gastrectomy. Multivariate logistic regression analyses were used with in-hospital mortality as the dependent variable to evaluate the effect of low, intermediate, and high hospital volume (average of ≤5, 6-20, and >20 gastric resections for cancer per year, respectively). Multivariate analyses were repeated in different subsets of patients to determine if hospital volume had variable effects on mortality depending on the subset evaluated.
RESULTS:
From 1998-2011, a total of 24,538 patients were included. The overall perioperative mortality rate was 5.5%, and multivariate analysis demonstrated that patients who received an operation in a center that performed a high-volume of gastric resections was protective (OR 0.64, 95% CI 0.50-0.81) when compared to patients who underwent surgery in a low-volume hospital. Other independent risk factors included male gender, age ≥65 years, Caucasian race, and Charlson Comorbidity Index (CCI) ≥3.
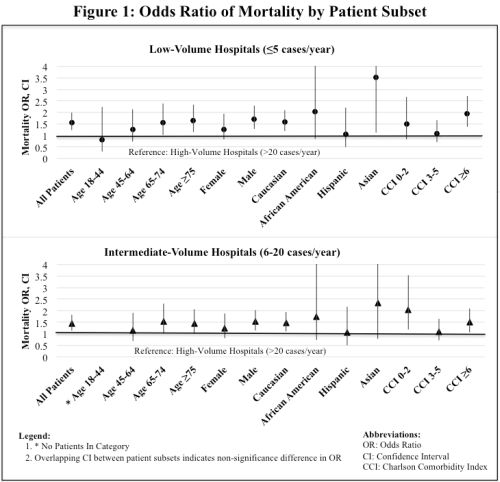
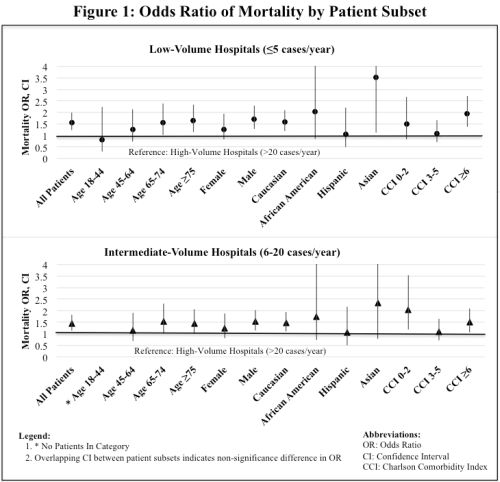
Upon subset analyses, there were no cohorts of patients that had a significantly lower risk of mortality if they received their operation in a low or intermediate-volume center when compared to a high-volume center. The risk of mortality for those undergoing surgery in low-volume hospitals was statistically significantly elevated in certain subsets (age ≥75, male, Caucasian, Asian, CCI ≥6) when compared to high-volume hospitals. Similarly, in intermediate-volume hospitals, mortality risk was significantly elevated in males, Caucasians, and those with CCI 0-2 and CCI ≥6. There were no significant differences in mortality between subgroups as evidenced by overlapping confidence intervals. (Figures 1A,B).
CONCLUSION(S):
There was no heterogeneity of treatment effect observed in gastric cancer patients undergoing surgery at low, intermediate, or high volume centers. These data support the current recommendation that all patients with gastric cancer should receive treatment at high-volume centers. This recommendation is particularly important for high-risk subgroups such as elderly patients and those with medical comorbidities.
Back to 2015 Annual Meeting Program
|