|
Back to 2015 Annual Meeting Program
BRAVO Wireless Esophageal pH Monitoring: a More Cost-Effective Approach Than Empiric Proton-Pump Inhibitor Therapy for Suspected Gastroesophageal Reflux Disease
Cheguevara Afaneh*1, Veronica Zoghbi1, Brendan M. Finnerty1, Anna Aronova1, Thomas Ciecierega2, Carl V. Crawford2, Thomas J. Fahey1, Rasa Zarnegar1
1Surgery, NY Presbyterian Hospital, New York, NY; 2Medicine-GI, NY Presbyterian Hospital, New York, NY
Introduction: Early referral for esophageal pH monitoring via transnasal catheter has been shown to be more cost-effective than empiric proton-pump inhibitor (PPI) therapy to diagnose gastroesophageal reflux disease (GERD); however, the relative cost-effectiveness may be negated by the variable sensitivity, inconvenience & discomfort. We hypothesize that early referral for BRAVO esophageal pH monitoring will also demonstrate substantial cost-savings compared to empiric PPI therapy given the superior sensitivity and comfort.
Methods: We reviewed 100 consecutive patients who underwent BRAVO esophageal pH monitoring with Demeester scoring for suspected GERD at our institution. Indications included both esophageal and extra-esophageal symptoms. A BRAVO cost model was generated based on the procedural cost and subsequent medical treatment dictated by the results. Calculations were performed assuming 75%, 85%, and 95% sensitivity of BRAVO esophageal pH monitoring. Cost savings analyses were performed for both esophageal & extra-esophageal symptoms. A cost equivalence calculation was performed to investigate how many weeks of empiric PPI therapy (low-dose generic PPI and high-dose name-brand PPI) would equate to the cost of BRAVO placement.
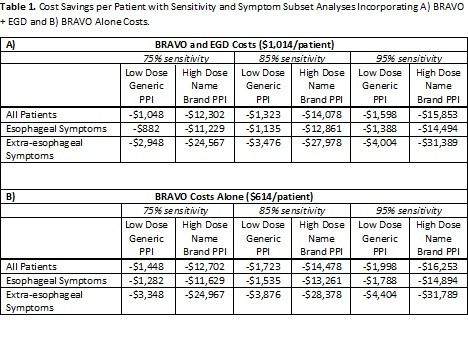
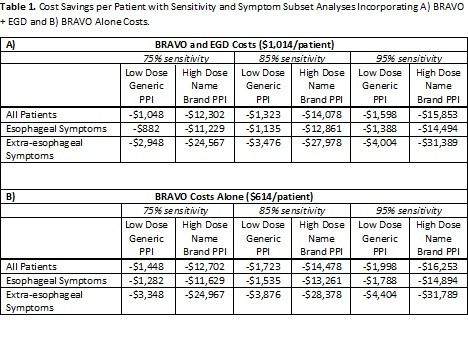
Results: Eighty-seven patients were available for analysis. Mean age was 50 ± 14.3 years and 67% of patients were female. The median number of weeks of PPI use prior to referral was 215 (range 0-520). Overall, 43 patients (49%) had BRAVO results diagnosing GERD; 98% had esophageal symptoms. For patients with negative BRAVO studies (51%), a median of 113 (0-520) weeks of unnecessary PPI therapy occurred. Assuming 75% sensitivity, estimated costs savings of early BRAVO placement compared to empiric therapy beyond 8 weeks were \,048 to \,302 per patient, for low-dose generic and high-dose name-brand PPI, respectively. For patients with extra-esophageal symptoms, cost savings ranged from \,948 to \,567 per patient (Table 1A). Assuming 95% sensitivity, estimated costs savings of early BRAVO placement ranged from \,598 to \,853 per patient. For patients with extra-esophageal symptoms, cost savings ranged from \,004 to \,389 per patient. Assuming all of these patients were to undergo endoscopy given their symptoms, we have included the cost savings tailored to only include the cost of BRAVO placement and analysis (Table 1B). The cost equivalence of PPI therapy to BRAVO placement is 36 weeks for low-dose generic PPI and 6 weeks for high-dose name brand PPI.
Conclusions: BRAVO testing is more cost-effective than prolonged empiric medical management for GERD. Given that most patients undergo EGD during the work-up for GERD, the placement of a BRAVO is a cost effective diagnostic modality when incorporated early in the treatment algorithm.
Back to 2015 Annual Meeting Program
|