|
Back to 2015 Annual Meeting Program
Adjunctive Multiple Rapid Swallows Increases Sensitivity of High Resolution Manometry in Patients With Dysphagia
Shunsuke Akimoto*, Se Ryung Yamamoto, Harit Kapoor, Tommy H. Lee, Sumeet K. Mittal
Department of Surgery, Creighton University Medical Center, Omaha, NE
Introduction
Patients with dysphagia are assessed with normal High Resolution Manometry (HRM) , the current gold standard. Recently, provocative Multiple Rapid Swallow technique (MRS) has been reported to provide additional detail in characterization of the esophageal transit. The aim of this study is to compare the test-characteristics of HRM with adjunctive MRS in the detection of patients with dysphagia.
Methods
All patients undergoing HRM evaluation between June 2014 to October 2014 were additionaly administered the MRS. Patients swallowed four 2ml water boluses, each four seconds apart. The parameters measured were Post-Deglutitory Inhibition(PDI) and the success of Rebound Esophageal Contraction(REC) using the 30mmHg isobaric contour. PDI was considered complete unless a contraction measuring > 3cm was identified, wherein it was considered incomplete. REC was considered failed when there was no smooth muscle contraction, the intersegmental trough was >3cm or when the contraction was interrupted for >3cm. We compared the sensitivity (Se), specificity (Sp), positive predictive value (PPV) and negative predictive value (NPV) of HRM alone and with adjunctive MRS in the detection of dysphagia. Patients with known achalasia or previous foregut surgery were excluded.
Results
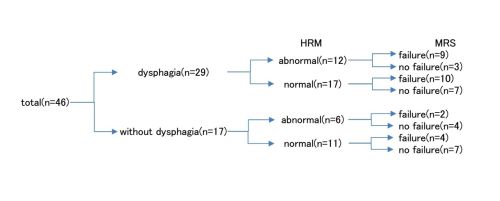
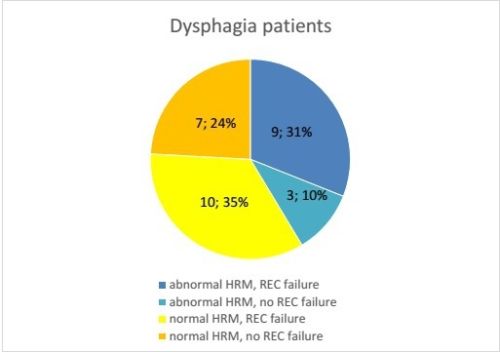
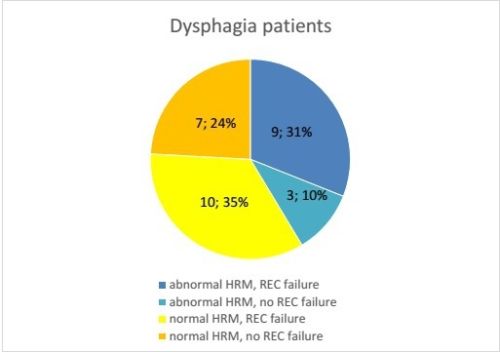
Sixty-five patients underwent HRM during the study period, of which 46 met the inclusion criteria. The mean age of the group was 57 years with 19 (41.3%) males. Twenty-nine (63%) patients had dysphagia. Those with and without dysphagia had similar mean age (57.2 vs. 56.7) and gender distribution (males%; 37.9% vs. 47.1%). On HRM, patients with and without dysphagia had similar Integrated relaxation pressures (IRP) (9.2 vs. 9.9; p=0.771) and Distal contractile integral (DCI) (2821 vs. 2552; p=0.671). In patients with dysphagia, REC failure (65.52%) was more common than abnormal PDI (37.9%) and outflow obstruction (IRP≧15) (13.8%). Patients with dysphagia had significantly higher rate of REC failure when compared to patients without dysphagia (65.5% vs. 35.3%; p=0.047) but PDI was not statistically different (37.9% vs. 23.5%; p=0.315). The Se, PPV and NPV of REC component of the test was much higher than the PDI component (Se; 65.5% vs. 37.9%, PPV; 76% vs. 73.3%; NPV: 52.4% vs. 41.9%). The Sp of the PDI component was marginally higher than that of the REC (76.5% vs. 64.7%). Overall, MRS, especially the REC component stood out as a better indication of dysphagia than conventional HRM alone (Se; 41.4%, Sp; 64.7%, PPV; 66.7%, NPV; 39.3%).
Conclusion
MRS seems to be a valuable adjunct in the evaluation of dysphagia. It identified an additional 10 patients as having abnormal motility which were missed by routine HRM. If incorporated into routine practice, we may be able to objectively detect about 50% more patients with dysphagia which remain undetected currently.
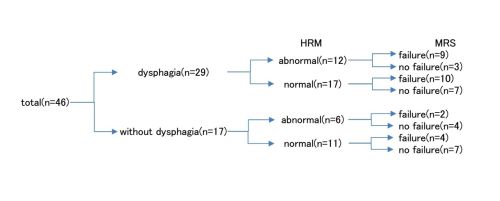
Flowchart illustrating subgrouping of study population based on symptoms and results of manometric testing
Back to 2015 Annual Meeting Program
|