|
 |
Back to 2015 Annual Meeting Program
Surgeon Volume Correlates With Reduced Mortality and Improved Quality in the Surgical Management of Diverticulitis
Rachelle N. Damle*1, Julie Flahive3, Jennifer S. Davids2, Justin a. Maykel2, W. Brian Sweeney2, Paul R. Sturrock2, Karim Alavi2
1Surgery, University of Masschusetts Medical School, Worcester, MA; 2Division of Colorectal Surgery, University of Masschusetts Medical School, Worcester, MA; 3Center for Outcomes Research, University of Masschusetts Medical School, Worcester, MA
Background: Surgeon volume is an important determinant of quality and cost outcomes. We evaluated the association between surgeon and hospital volume and outcomes in the operative management of acute diverticulitis.
Methods: We performed a retrospective study of patients who were admitted with diverticulitis using the University HealthSystem Consortium Clinical Database from 2008-2012. Outcomes evaluated included use of a minimally invasive surgical approach, stoma creation, intensive-care unit admission, post-operative complications, length of stay, readmissions, mortality, and total direct hospital costs by surgeon-volume. Surgeon-volume was categorized according to Very-High (VHVS) (>31), High (HVS) (13-31), Medium (MVS) (6-12), and Low (LVS) (≤5) average annual volumes.
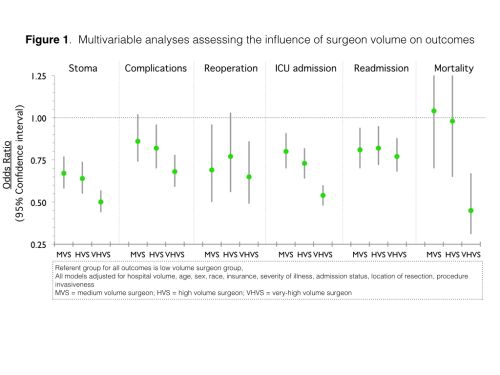
Results: Over the study period, 19,212 patients with a mean age of 59 years, 54% female makeup, and 55% rate of private insurance met inclusion criteria. Similar to the unadjusted analysis, multivariable analysis revealed decreasing odds of stoma creation, complications, ICU admission, reoperation, readmission, and inpatient mortality with increasing surgeon volume (Figure 1). Additionally, compared with the LVS group, higher surgeon volume was associated with significantly higher rates of minimally invasive approach (MVS OR 1.52 95%CI 1.35-1.72, HVS 1.80 95%CI 1.61-2.02, VHVS 2.35 95%CI 2.11-2.61). Median length of stay and costs were also notably lower with increasing surgeon volume (Table 1).
Conclusions: Quality, as defined by decreased complications, stoma rates, readmissions, and mortality, is tightly associated with volume. These differences do not appear to be explained by the urgency of the procedure. Higher volume surgeons appear more likely to use minimally invasive techniques. Given the complex issues in management and increased oversight by third party payers for quality service, strong consideration should be given to referral to high volume surgeons.
TABLE 1. Multivariable analyses assessing the influence of surgeon volume on length of stay and cost (referent group for all models is low volume surgeon group)
| MVS | HVS | VHVS | | Length of Staya (days) | -0.35
(-0.65, -0.05) | -0.58
(-0.87, -0.30) | -1.21
(-1.47, -0.94) | | Total Direct Hospital Costa (\0 | -2267
(-2959, -1576) | -2346
(-3009, -1682) | -3643
(-4246, -3040) | All values shown are beta-coefficient (95% CI)
|
aModel adjusted for: hospital volume, age, sex, race, insurance, severity of illness, admission status, location of resection, minimally invasive vs. open approach 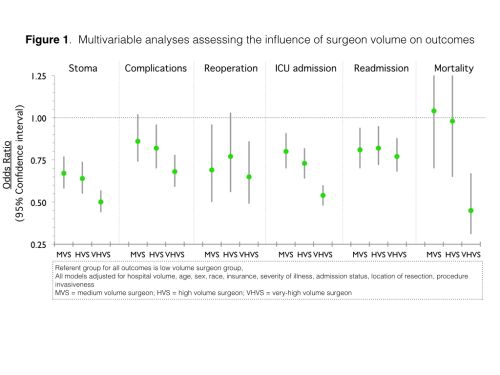
Back to 2015 Annual Meeting Program
|